Continuous positive airway pressure (CPAP) is the most common therapeutic modality for obstructive sleep apnoea (OSA). However, deciding whether a patient should be treated with CPAP is not a simple process, in light that a large number of complex clinical variables need to be considered in the decision process.1 This difficulty is particularly apparent among mild–moderate OSA patients, since quality of life is scarcely affected, CPAP compliance is relatively low, and treatment effectiveness is unclear.2–4 Although setting a threshold in the apnea–hypopnea index (AHI) is the most usual criterion for CPAP prescription in OSA, current clinical guidelines do not provide the treating physician with unambiguous rules. Consequently, virtually universal disagreement in decision making about implementation of CPAP therapy5 has been considered as inevitable. In fact, a conventional consultation process among physicians evaluating OSA patients is viewed as impractical and not routinely implementable considering the high prevalence of OSA,6 therefore resulting in a considerable number of patients being then referred for initiation of CPAP therapy.7 However, consultation among colleagues can be markedly facilitated and become cost-effective using telematics.8 Nevertheless, this approach has not been used until now to improve decision-making in CPAP prescription.
We herein describe a novel model of telematic physician consultation (TPC) in the context of decision making regarding the need for CPAP therapy, and use real-world data to provide a proof of concept of its feasibility and potential benefits. In TPC, the physician who treats a patient has the external support of 2 independent specialists to decide on CPAP treatment. While this approach seems straightforward and reasonable, whether it is feasible and improves decision-making in routine OSA patients has not been assessed. To this effect, we randomly selected 40 patients with mild–moderate OSA (AHI<40events/h) from the database of a clinical trial (NCT02779894; ClinicalTrials.gov) that included a general population of patients with OSA.9 All the clinical and sleep study variables (≈60) of each patient were placed anonymously on a specially designed website that was only accessible to 6 experienced sleep physicians from different Spanish hospitals, who were then asked to provide their recommendations about CPAP prescription: ‘yes’ or ‘no’ (‘no’ could be both a clear negative to CPAP or no prescription until additional patient evaluation). For each possible combination of ‘yes’–‘no’ recommendations we first theoretically calculated the probability of correct decision when the latter was made by 1 or 3 physicians; second, we experimentally determined how the ‘yes’–‘no’ recommendations were distributed among the patients, and finally we computed the expected value of correct decision corresponding to 1- or 3-physician decision on CPAP initiation.
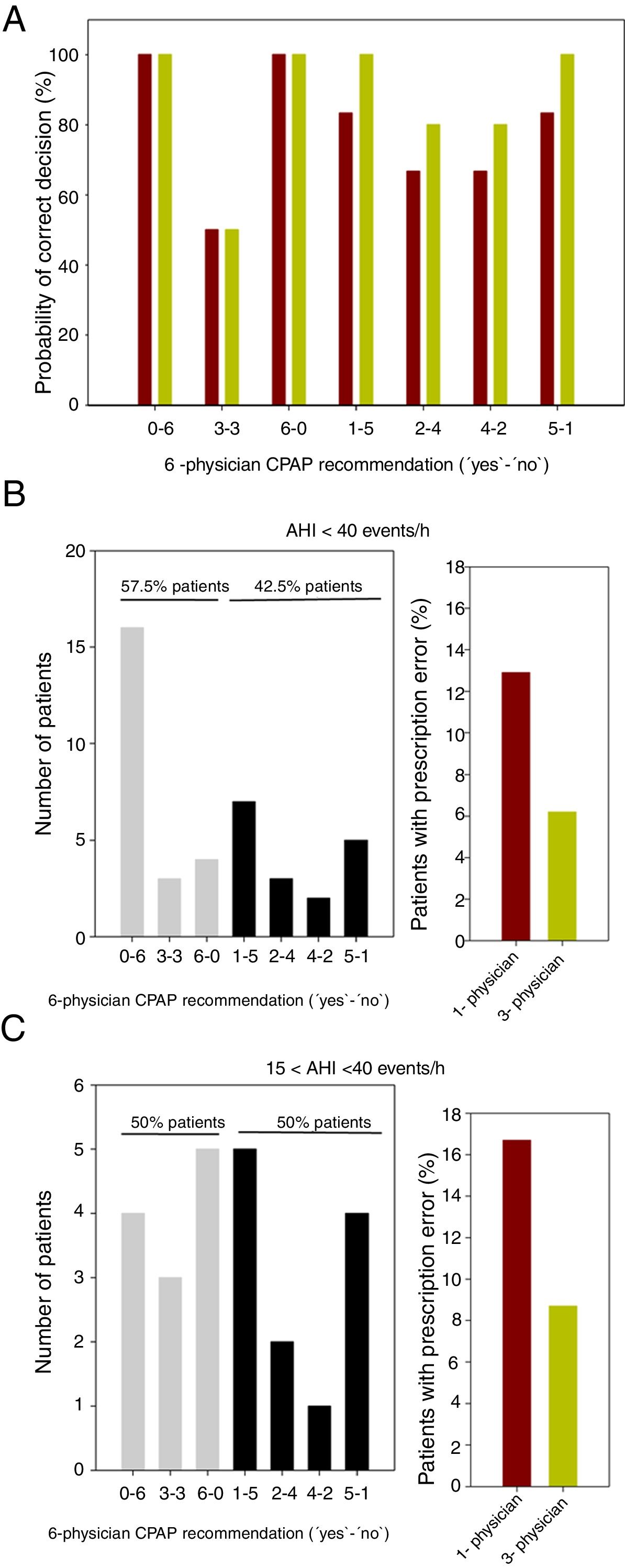
As the correct decision for each patient is unknown, we assumed that it was better estimated by the majority of the recommendations of the 6 physicians. Consequently, among the 7 possible ‘yes’–‘no’ recommendations (0–6, 1–5, 2–4, 3–3, 4–2, 5–1 and 6–0), the decision on CPAP treatment was considered correct only for recommendations 4–2, 5–1 and 6–0. For each of the 7 combinations ‘yes’–‘no’, the probability that a single physician would recommend the correct decision is 6/6, 5/6, 4/6, 3/6, 4/6, 5/6 and 6/6 (i.e. 100%, 83.3%, 66.7%, 50%, 66.7%, 83.3% and 100%), respectively (Fig. 1A). To calculate the probability of a correct CPAP prescription decision when taken by the majority of 3 physicians, we considered that among the 20 different possible combinations of 3 recommendations from 6 physicians (C(6,3)=6!/(3!(6−3)!), the number of combinations that yields a positive result (2 or 3 physicians recommending CPAP) are 0, 0, 4, 10, 16, 20 and 20 for the above 7 ‘yes’–‘no’ recommendations, respectively. Therefore, the probability of correct decision is: 100%, 100%, 80%, 50%, 80%, 100% and 100%, respectively (Fig. 1A). As expected, only when the 6-physician recommendation is unanimous (0–6 or 6–0) or when it is a tie (3–3) there is no statistical advantage when the decision is made by 3 or 1 physicians. Otherwise, decision-making by 3 physicians instead of 1 physician alone increases the correct decision probability (Fig. 1A).
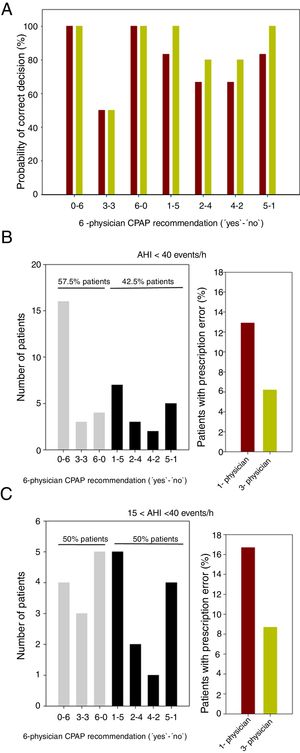
(A) Probability of correct CPAP prescription when the decision is taken by 1 physician (brown columns) or by a 3-physician group (green columns), for the different 7 possible (‘yes’–‘no’) recommendations from 6 physicians (0–6, 1–5, 2–4, 3–3, 4–2, 5–1 and 6–0). In case of unanimous (0–6 or 6–0) or draw (3–3) recommendations there is no statistical advantage when the decision is taken from 3 or 1 physicians. In the other cases, 3-physician decision is advantageous as compared with 1-physician decision. (B) Left: Distribution of 6-physician recommendations for the 40 patients with mild–moderate OSA (AHI<40events/h). Gray: recommendations resulting in no statistical advantage when the decision is made by 3 or 1 physicians; Black: recommendations for which decision-making by 3 instead of 1 physician increases correct decision probability. Right: Expected error in CPAP prescription when the decision is taken by 3 physicians (green column) instead 1 physician (brown column). (C) Same as in (B) but only for moderate OSA patients (15<AHI<40 events/h).
To calculate the real-life impact in the decision-making of 1 or 3 physicians, the theoretical probability analysis in Fig. 1A was combined with the actual distribution of the spectrum of real-data recommendations of the 6 external physicians on the 40 mild–moderate OSA patients (a total of 240 decisions), shown in Fig. 1B. The left panel in this figure reflects the variability in physician agreement as regards therapeutic decision on CPAP.9 In 42.5% of the patients, the 6-physician recommendation was one for which using the 3-physician decision approach reduces the prescription error versus the 1-physician approach (Fig. 1A). When considering the actual distribution of the recommendations (Fig. 1B) and the corresponding probability of correct decisions (Fig. 1A), the error frequency in CPAP prescription decision would be considerably reduced from 12.9% to 6.2% of the patients (Fig. 1B). Interestingly, when the analysis was limited to the 24 patients with moderate OSA (15<AHI<40events/h), the decision-making error when switching from 1-physician to 3-physician prescription was also reduced by ≈50%: from 16.7% to 8.7% of patients (Fig. 1C).
This study provides a solid proof of concept on the feasibility and potential improvements achieved by our novel proposal of telematic multi-physician decision-making approaches for improving CPAP treatment decision in OSA. If the attending physician is supported by the opinion of 2 independent colleagues, unnecessary CPAP prescription may be avoided in ≈8% of mild–moderate OSA patients. Such changes in clinical decision would have a considerable impact both in cases in which CPAP was prescribed to patients not requiring the treatment (patient inconvenience and unnecessary treatment costs (≈320US$/year10) and in cases where patients requiring CPAP would not be treated (reducing adverse health consequences of untreated OSA and associated opportunity costs (2700–5200US$/year11). Considering that the incidence of new CPAP prescriptions is ≈25 per 10,000 inhabitants per year,7 and that in ≈70% of OSA patients the disease is mild–moderate,6 it can be estimated that TPC, if implemented as proposed here, would avoid prescription errors in ≈175,000 patients per year in the OCED countries (1.25 billion inhabitants), likely resulting in beneficial reductions in healthcare costs, even after TPC implementation. Indeed, the increases in the effectiveness of CPAP prescription would entail only very modest cost increments per patient, corresponding to ≈15min of off-line telematic assessment by 2 sleep specialists.
In conclusion, the implementation of an updated telematic version of the consultation among physicians could provide considerable cost-effective improvements in the prescription of CPAP in OSA, a proposal that we believe should be substantiated in the future by specifically designed clinical trials including a wide-spectrum population to provide statistically powered conclusions. Notably, the approach described here can be readily transposed to other unresolved issues in OSA diagnosis and treatment,12 in which complex decision-making could benefit from a straightforward approach of inter-physician consultation.
FinancialSupported in part by the Spanish Ministry of Economy and Competitiveness (SAF2017-85574-R, DPI2017-83721-P; AEI/FEDER, UE), and the CERCA Program of Generalitat de Catalunya. D.G. is supported by NIH grant HL130984.