Systemic sclerosis (SSc) is a rare disease, characterized by complex immune disorders, vascular damage and fibrosis of the skin and visceral organs.1 Autoimmune (AI) diseases, including SSc, and immunosuppressive drugs have been associated with many types of cancers.
Kaposi's sarcoma (KS) is a rare angioproliferative tumor associated with human herpesvirus 8 (HHV-8) infection. Mucocutaneous involvement is the most common, but KS can be seen in almost all visceral sites.2 Pulmonary KS can involve the lung parenchyma, airways, pleura, and/or intrathoracic lymph nodes.3 The iatrogenic type, one of the four KS types, is related to immunosuppressive therapy, typically in patients that have undergone solid organ transplantation or with other conditions such as AI diseases.2
We report the case of a 66-year-old woman, diagnosed with limited cutaneous SSc at the age of forty, with a four-year history of pulmonary involvement presenting as interstitial lung disease with an usual interstitial pneumonia pattern. She was being treated with pentoxifylline 1200mg/day, pantoprazole 40mg/day, azathioprine 100mg/day (2mg/kg/day) and prednisolone 10mg/day.
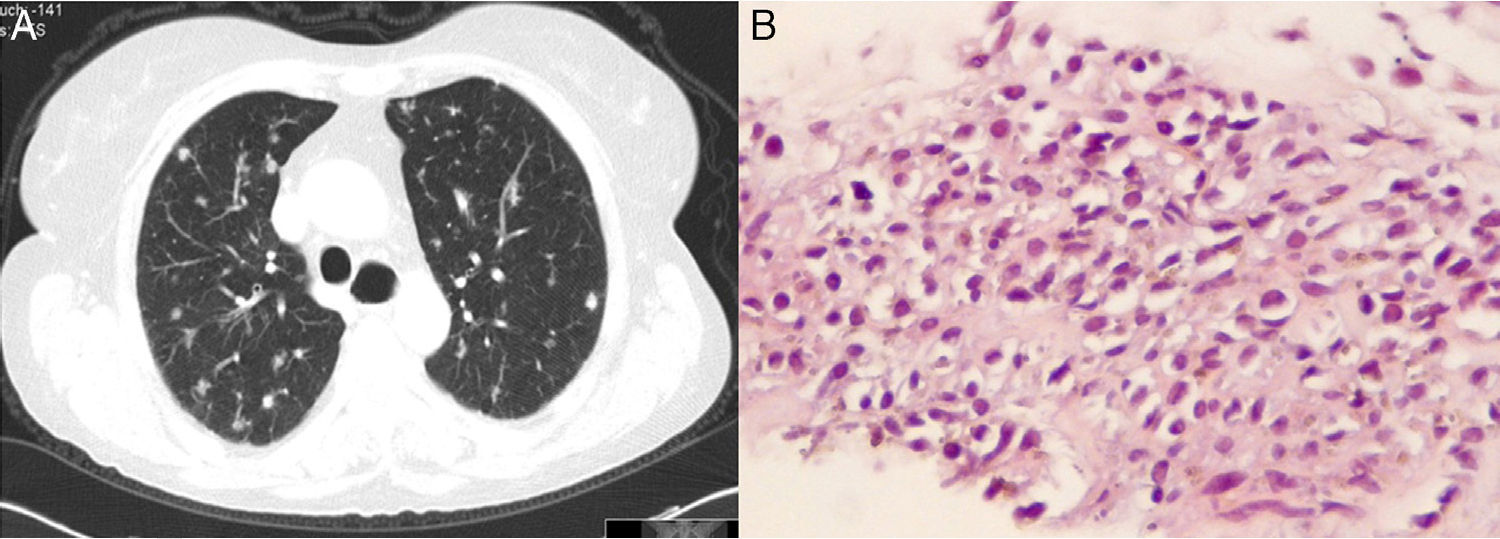
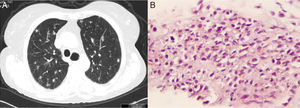
The patient presented a brownish-to-reddish de novo nodule on her lower right eyelid that was surgically removed, and which histological examination was compatible with KS. Serology for human immunodeficiency virus (HIV) was negative. Six months later, the patient presented some violaceous nodular lesions on her back, abdominal area and upper thigh, and reported worsening of respiratory symptoms, with more cough and nonpurulent sputum. She underwent high-resolution chest computed tomography that showed new multiple subcentimeter pulmonary nodules, diffusely dispersed throughout both lungs (Fig. 1A). Routine laboratory tests showed no significant changes, and lymphocyte subpopulations on a peripheral blood sample were normal. Repeat HIV serology was again negative. Bronchofibroscopy with bronchoalveolar lavage was performed, revealing intense lymphocytosis, expected in the context of pulmonary involvement of SSc, but with negative microbiological examination and no signs of malignancy. A transthoracic needle biopsy of one of the pulmonary nodules was then carried out, and the histology showed characteristic spindle cells compatible with KS diagnosis (Fig. 1B). The latency-associated nuclear antigen (LANA-1) was not tested, but KS diagnosis was confirmed by HHV-8 DNA detected by polymerase chain reaction. Immunosuppressive therapy was adjusted to exclude azathioprine. The KS lesions remained stable and the patient was closely followed-up to detect progression of KS, which would have been treated with chemotherapy.
To our knowledge, this is the first case of Kaposi's sarcoma with pulmonary involvement in a patient with SSc. Patients with SSc have been shown to have a higher prevalence of genetic damage that predisposes to carcinogenesis.1 Lung and hematological malignancies are more closely associated with SSc.1
KS has a very low incidence in patients with AI diseases.4,5 However, it appears that the presence of an AI disease is in itself a risk factor for the development of KS, as some cases without prior immunosuppressants have been reported.5
Furthermore, KS is known to be induced or triggered by immunosuppressive therapy in patients previously infected with HHV-8,4,5 although no relationship between type, duration or required dosage has been established.4 Studies have also shown that immunosuppression-related KS tends to be aggressive, with more frequent visceral involvement.4
In this case, the patient had been treated with a long-term combination of steroids with azathioprine, and had the particularity of presenting cutaneous and pulmonary KS. The extent to which pulmonary manifestations were associated with the presence of pulmonary involvement related to SSc is unknown, but there could be a link.
In this context, the occurrence of KS in the absence of other predisposing factors, namely HIV infection, was interpreted to be treatment and/or disease related.
With regard to the management of these patients, modification, reduction or withdrawal of the immunosuppressive medication should be attempted, as this will result in KS remission in about 50% of cases, while radiotherapy and/or chemotherapy may be needed in refractory or more severe cases.5
Please cite this article as: Aguiar F, Araújo D, Brito I. Esclerosis sistémica y sarcoma de Kaposi con afectación pulmonar: una asociación inesperada. Arch Bronconeumol. 2017;53:165–166.