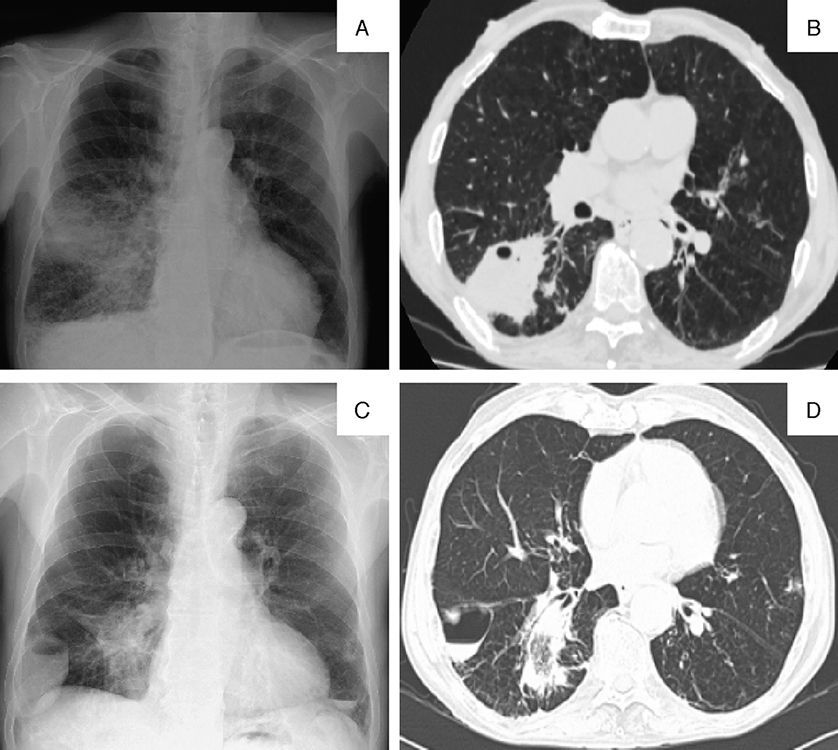
A 70-year-old man, smoker, with no significant medical history, was admitted to the pulmonology department with a 3-month history of moderate exertional dyspnea associated with fatigue. He reported productive cough with expectoration of mucus. He denied hemoptysis and constitutional symptoms. Lung auscultation revealed decreased breath sounds on the right side. Blood analyses showed elevated systemic inflammatory markers. Chest X-ray (Fig. 1A) revealed an opacity in the right lung associated with a micronodular pattern. Chest CT (Fig. 1B) showed a consolidation in the right lower lobe (RLL) with initial cavitation. Bronchoscopy showed no endobronchial lesions and microbiological study of aspirate only revealed a methicillin-resistant Staphylococcus aureus. Despite targeted antibiotic therapy, clinical and radiological progress were poor, and chest X-ray (Fig. 1C) showed an opacity and a new cavitary lesion; chest CT (Fig. 1D) confirmed consolidation with cavitation and a cystic formation compatible with pneumatocele. A parenchymal lesion biopsy was consistent with organizing pneumonia (treated with prednisone 0.75mg/kg/day for 4 weeks, which was then progressively tapered). Clinical and radiological progress was good. During follow-up, resolution of the pneumatocele lesion was observed.
(A) Initial chest X-ray (posteroanterior [PA]): heterogeneous opacity in the right lung associated with a micronodular pattern. (B) Initial chest computed tomography (CT) (axial plane [AP]): consolidation in the apical segment of the RLL with initial cavitation. (C) Chest X-ray (PA): triangular opacity and a new cavitary lesion, with air-fluid level, occupying the right costophrenic angle. (D) Chest CT (AP): consolidation with cavitation in the apical segment RLL, and cystic formation with air-fluid level, consistent with pneumatocele.
Please cite this article as: Gomes R, Fernandes F, Luís F. Neumatocele y neumonía organizada sincrónicos en el curso de una infección por Staphylococcus aureus. Arch Bronconeumol. 2016;52:561


![(A) Initial chest X-ray (posteroanterior [PA]): heterogeneous opacity in the right lung associated with a micronodular pattern. (B) Initial chest computed tomography (CT) (axial plane [AP]): consolidation in the apical segment of the RLL with initial cavitation. (C) Chest X-ray (PA): triangular opacity and a new cavitary lesion, with air-fluid level, occupying the right costophrenic angle. (D) Chest CT (AP): consolidation with cavitation in the apical segment RLL, and cystic formation with air-fluid level, consistent with pneumatocele. (A) Initial chest X-ray (posteroanterior [PA]): heterogeneous opacity in the right lung associated with a micronodular pattern. (B) Initial chest computed tomography (CT) (axial plane [AP]): consolidation in the apical segment of the RLL with initial cavitation. (C) Chest X-ray (PA): triangular opacity and a new cavitary lesion, with air-fluid level, occupying the right costophrenic angle. (D) Chest CT (AP): consolidation with cavitation in the apical segment RLL, and cystic formation with air-fluid level, consistent with pneumatocele.](https://static.elsevier.es/multimedia/15792129/0000005200000011/v1_201610250037/S1579212916000665/v1_201610250037/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w98FxLWLw1xoW2PaQDYY7RZU=)








