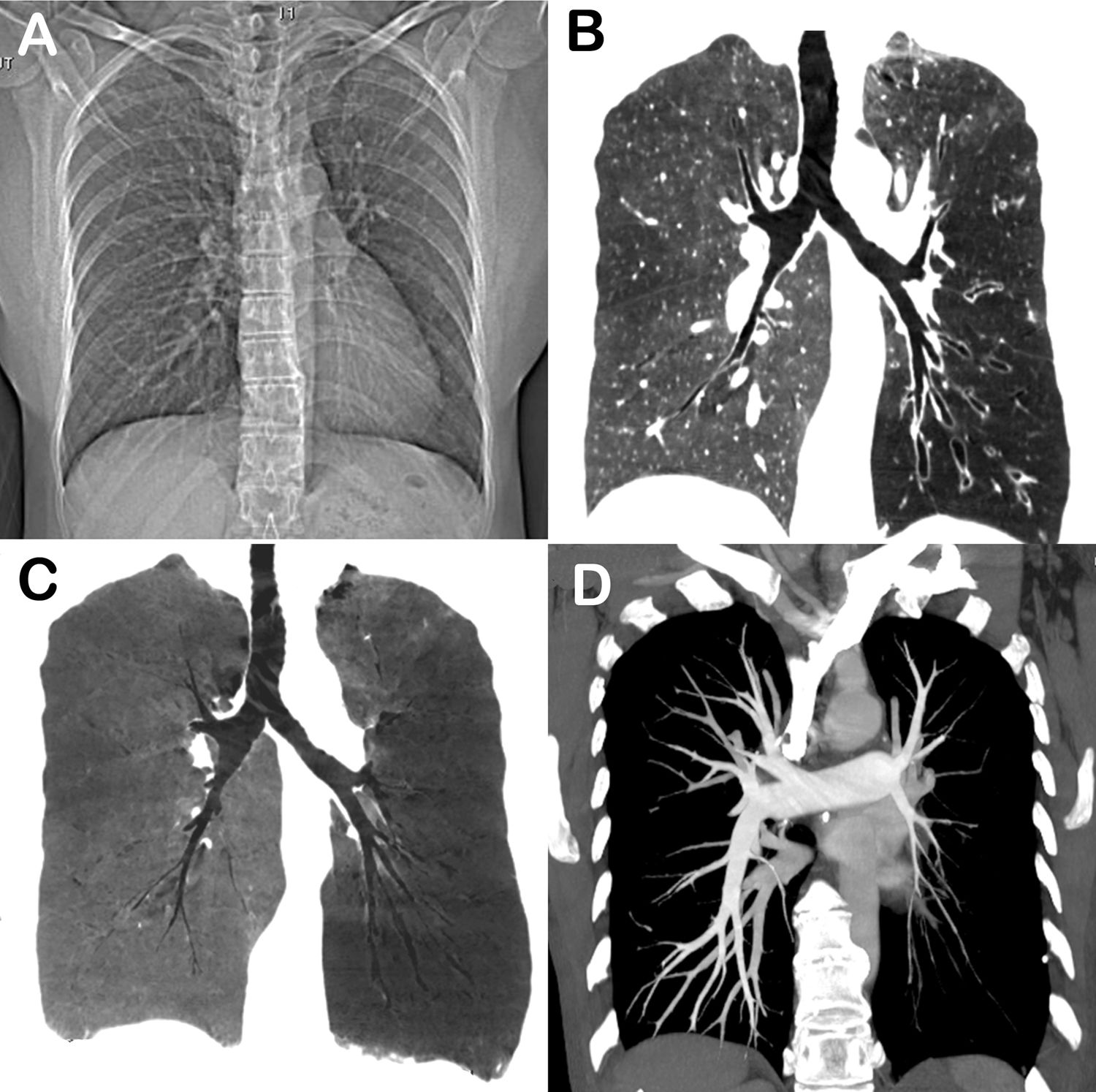
A 51-year-old non-smoking woman presented to the emergency department with progressive exertional dyspnea and productive cough. She had a history of recurrent pulmonary infections since childhood. Laboratory test findings were unremarkable. Chest radiography revealed volume loss in the left hemithorax, with mediastinal homolateral deviation and expiratory air trapping. Chest CT demonstrated a decrease in the volume and attenuation of the left lung, with bronchiectasis in the left lower lobe, and hypoplasia of the left main pulmonary artery and its branches (Fig. 1). Bronchoscopy findings were normal, and the bronchoalveolar lavage fluid was negative for neoplastic cells, acid-fast bacilli, and fungi. Based on the clinical history and imaging findings, the diagnosis of Swyer-James-McLeod syndrome (SJMS) was established.
(A) CT scout image in inspiration showing reduced lung volume on the left side, with homolateral displacement of the mediastinum. Chest CT coronal reconstructions with maximum-intensity (B) and minimum-intensity (C) projections demonstrate diffuse decreased density of the left lung, with bronchiectasis in the lower lobe. (D) Angio-CT image showing hypoplasia of the left pulmonary artery and its branches.
SJMS is an acquired disease secondary to viral bronchiolitis and pneumonitis that occurs during childhood, with concomitant vasculitis.
It is most frequently diagnosed in children, although some patients are diagnosed only in adulthood. Patients may be asymptomatic or present with dyspnea, cough, hemoptysis, and recurrent pulmonary infections. The diagnosis of SJMS is based on imaging findings of decreased volume and density of the affected lung, with displacement of the mediastinum to the affected side, and hypoplasia of the pulmonary artery and its branches. Other findings may include bronchiectasis and air trapping.1,2
Conflicts of interestThe authors declare that they have no conflicts of interest to express.