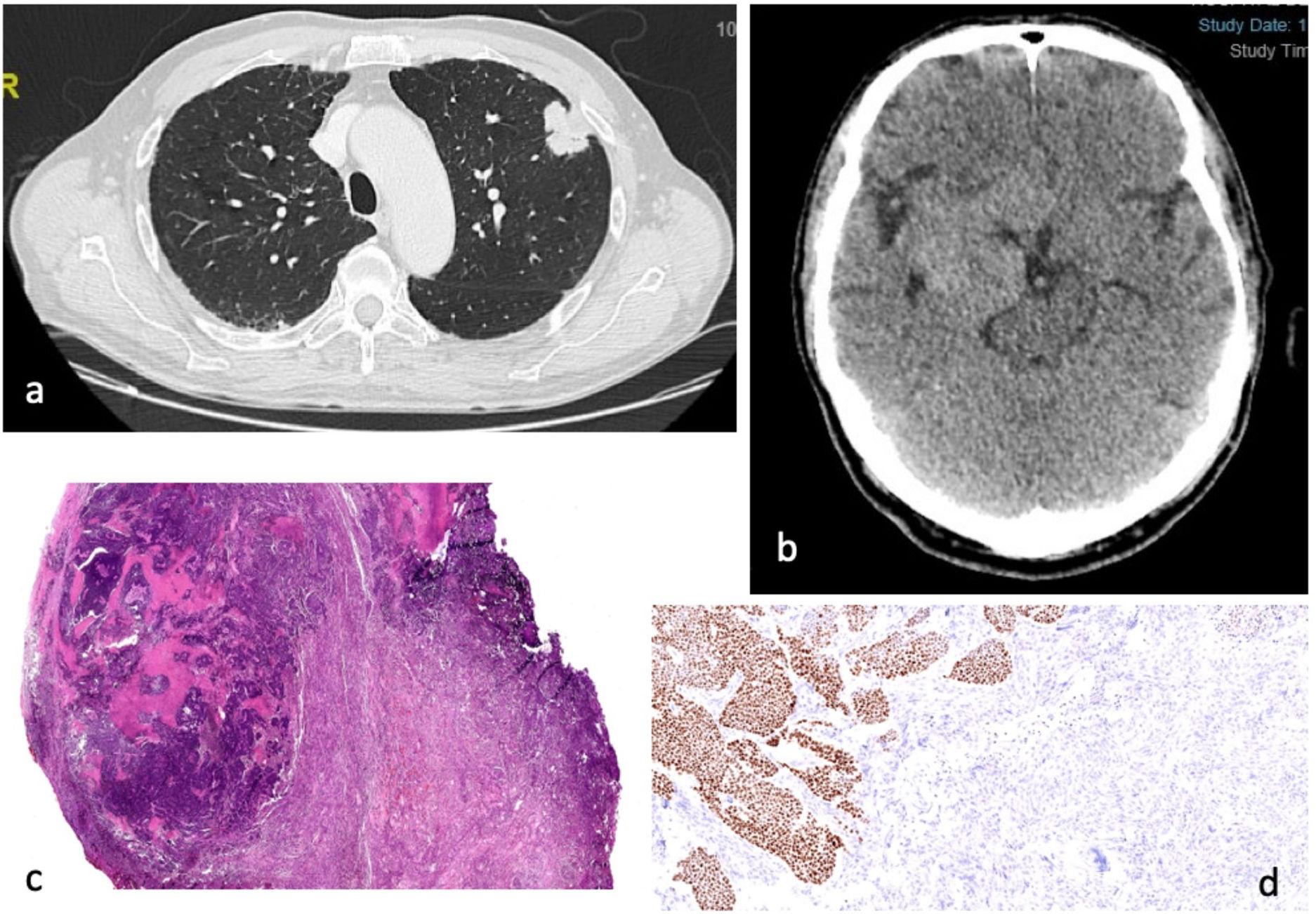
We present a 71-year-old male, former smoker of 40 cigarettes/day, operated from bladder adenocarcinoma in 2008, free of disease to date. Admitted to the hospital in December 2021 for seizures. He had two previous episodes months before without further study. No respiratory symptoms were associated. After hospitalization the study was completed and the cranial CT (Fig. 1b) revealed a hyperdense intracranial extra-axial mass adjacent to the right frontal and temporal lobes deviating the central line compatible with a meningioma, and a left pulmonary mass was found later in the X-ray. The thorax CT revealed a pulmonary mass in the left upper lobe (LUL) (Fig. 1a) contacting the pleura, without hiliar nor mediastinal enlarged lymph nodes. PET-CT was done, and endobronchial ultrasound ruled out lymphatic node infiltration. Core needle biopsy of the lung was insufficient for the diagnosis. After management agreement by a multidisciplinary team, the patient underwent a LUL VATS lobectomy in May 2022. Pathology results were compatible with squamous lung cell carcinoma.
(a) Thorax CT axial contrast-enhanced: 33mg lung spiculated mass located in the upper left lobe contacting and thickening the visceral pleura (T2a). (b) Cranial CT axial, unenhanced: large right-sided extra-axial mass of 55mm, hyperdense, compressing right cerebral peduncule and closely related to arterial vascular structures. (c) HE stain 10×; poorly delimited basaloid cell nodule with areas of necrosis over a proliferation of spindle cells corresponding to meningioma (squamous carcinoma). (d) Immunohistochemistry P40 100×; epithelial cells from squamous carcinoma show P40 nuclear positivity while spindle meningeal cells are p40 negative.
A craniectomy with lesion excision was done in November 2022, and pathology reported squamous lung cell metastasis inside a meningioma tumour (Fig. 1c and d).
Massive sequencing (NGS) from both tumours was done in DNA and RNA, detecting a single nucleotide change in FGFR3 p.(R248C), and also copy numbers variations in PIK3CA and CDJN2A supporting the diagnosis of primary lung tumour with metastasis to meningioma.
After the surgery the patient suffered from secondary hydrocephalus and needed a ventriculoperitoneal shunt. During the follow-up in January 2023 in a CT hepatic lesions were found compatible with disease extension and chemotherapy was initiated, unfortunately the patient died due to progression a few months later.
The occurrence of metastases of malignant tumours into cranial tumours, known as “tumour-into-tumour” phenomenon is unusual although has been described decades ago, and has occasionally has been reported in the literature.1 The most common tumours in the brain are metastasis, and meningioma is the most common primary brain tumour, which is usually benign and arises from the meninges in the CNS.1,2 The area of meningioma is very rich in perfusion so it could be a target for metastatic spreading from other cancers. As available in the literature, the origin of metastatic neoplasm in 33.56% is breast cancer, 28% lung, 8.72% renal and 7.38% prostate tumours, less frequent being gastrointestinal, haematological, lymphomas or melanomas. Metastasis in 98% are from haematogenous origin. In 36.69% the tumour-to-meningioma metastasis was the first sign of cancer and 53.63% of patients had a previously diagnosed neoplasm.2
Tumour-to-meningioma metastasis is infrequent but should be considered as a diagnosis in patients with active cancer who develop neurological symptoms and have a newly diagnosed meningioma, but also in those considered in cancer remission in which a meningioma arises.2,3 Cancers that metastasize to meningiomas are not the same that usually metastasize to the brain.2
Conflict of InterestsThe authors state that they have no conflict of interests.