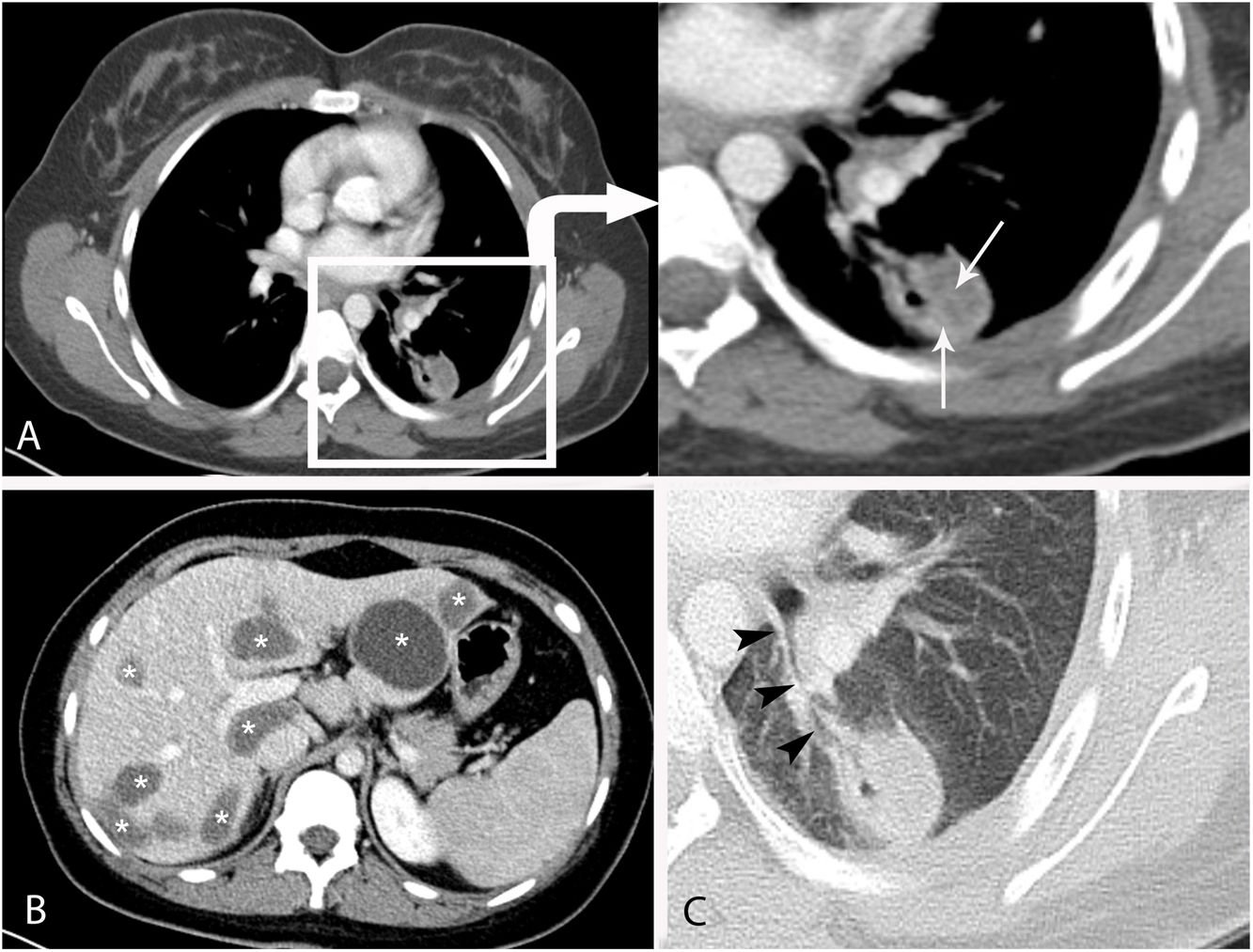
A 22-year-old female presented with complaint chest pain and abdominal pain. Contrast-enhanced thoracoabdominal computed tomography (CT) showed some well circumscribed heterogeneous nodules in the lung. And multiple cystic lesions were also seen in the liver (Fig. 1B) An echinococcus hemagglutination test was positive and hydatid cyst was considered. The patient was started oral albendazole treatment and was planned PAIR (puncture-aspiration-injection-reaspiration) treatment for liver and surgical treatment for lung after albendazole treatment. But two days later, before surgical treatment, she was admitted to the emergency department with a complaint of yellowish hemoptysis containing membranes. When the patient applied to the emergency service, her hemoptysis had already stopped spontaneously. The patient described a hemoptysis of about 60ml. Therefore, the cause of hemoptysis was investigated. There was no trauma history. Contrast-enhanced chest CT demonstrated a nodule with a heterogeneous density and an air bubble inside in the left lower lobe which was communication with a bronchial branch (Fig. 1A,C). The patient was surgically treated with cystectomy and 10mg/kg/day albendazole treatment was prescribed. Finally, pulmonary hydatid cyst was confirmed by surgery. The patient was diagnosed with spontaneous endobronchial rupture of pulmonary hydatid cyst.
Contrast-enhanced axial computed tomography (A) showed a heterogeneous nodule in the lower lobe of the left lung with air bubbles and internal germinative membranes (arrows). There was an increase in cyst density due to germinative membranes. Computed tomography (B) showed multiple well circumscribed hypodens hydatid cystic lesions in the liver (Asterisks). Computed tomography, lung window(C) showed the communication between the cyst and a bronchus (arrowheads).
Hydatid disease is a rare disease in human which occurs by the larvae of the Echinococcus. The disease is transmitted by contamination of food and water. Hydatid disease commonly involves the liver and lungs.1 The clinical presentation of the disease is non-specific. The diagnosis is confirmed by radiology supplemented with serology. The detection of germinative membrane on CT is diagnostic in the diagnosis of hydatid cyst.2 In addition, the presence of calcification may help in diagnosis.2 The presence of air bubbles is an important finding for the diagnosis of cyst rupture.2 The treatment of pulmonary hydatid cyst is either medical and/or surgical.3
Conflict of interestThe authors declare that they have no conflict of interest to the publication of this article.