Our study sought to know the current implementation of video-assisted thoracoscopic surgery (VATS) for anatomical lung resections in Spain. We present our initial results and describe the auditing systems developed by the Spanish VATS Group (GEVATS).
MethodsWe conducted a prospective multicentre cohort study that included patients receiving anatomical lung resections between 12/20/2016 and 03/20/2018. The main quality controls consisted of determining the recruitment rate of each centre and the accuracy of the perioperative data collected based on six key variables. The implications of a low recruitment rate were analysed for “90-day mortality” and “Grade IIIb-V complications”.
ResultsThe series was composed of 3533 cases (1917 VATS; 54.3%) across 33 departments. The centres’ median recruitment rate was 99% (25–75th:76–100%), with an overall recruitment rate of 83% and a data accuracy of 98%. We were unable to demonstrate a significant association between the recruitment rate and the risk of morbidity/mortality, but a trend was found in the unadjusted analysis for those centres with recruitment rates lower than 80% (centres with 95–100% rates as reference): grade IIIb-V OR=0.61 (p=0.081), 90-day mortality OR=0.46 (p=0.051).
ConclusionsMore than half of the anatomical lung resections in Spain are performed via VATS. According to our results, the centre's recruitment rate and its potential implications due to selection bias, should deserve further attention by the main voluntary multicentre studies of our speciality. The high representativeness as well as the reliability of the GEVATS data constitute a fundamental point of departure for this nationwide cohort.
Nuestro estudio buscó conocer el grado de implementación actual de la cirugía toracoscópica asistida por video (VATS, por sus siglas en inglés) para las resecciones pulmonares anatómicas en España. Presentamos nuestros resultados iniciales y describimos los sistemas de auditoría desarrollados por el grupo español de VATS (GEVATS).
MétodosRealizamos un estudio de cohortes prospectivo multicéntrico que incluyó pacientes que fueron tratados con resecciones pulmonares anatómicas entre el 20/12/2016 y el 20/03/2018. Los controles de calidad principales consistieron en determinar la tasa de reclutamiento de cada centro y la precisión de los datos perioperatorios recolectados en base a seis variables clave. Se analizaron las implicaciones de una baja tasa de reclutamiento para “mortalidad a los 90 días” y “complicaciones de grado IIIb-V”.
ResultadosLa serie estaba compuesta por 3533 casos (1917 VATS; 54,3%) en 33 servicios. La mediana de la tasa de reclutamiento de los centros fue del 99% (p25-p75: 76-100%), con una tasa de reclutamiento global del 83% y una precisión de los datos del 98%. No pudimos demostrar una asociación significativa entre la tasa de reclutamiento y el riesgo de morbi-mortalidad, pero se encontró una tendencia en el análisis no ajustado para aquellos centros con tasas de reclutamiento inferiores al 80% (usando los centros con tasas de 95-100% como referencia): OR=0,61 para el grado IIIb-V (p=0,081), OR=0,46 para la mortalidad a los 90 días (p=0,051).
ConclusionesMás de la mitad de las resecciones pulmonares anatómicas en España se realizan a través de VATS. Según nuestros resultados, la tasa de reclutamiento del centro y sus posibles implicaciones debido al sesgo de selección, deberían recibir más atención por parte de los principales estudios multicéntricos voluntarios de nuestra especialidad. La alta representatividad y la confiabilidad de los datos de GEVATS constituyen un punto de partida fundamental para esta cohorte nacional.
Because of improvements in the computerisation, management, and exploitation of clinical data systems, an increasing number of thoracic surgery studies have been derived from population databases or large multicentre registries. In this sense, the classic paradigm of a limited and often insufficient number of patients is being replaced by the greater need to examine the quality and reliability of our data.1 Even within our specialty, the number of studies attempting to analyse and publicise the quality of their recorded data has become exceptional.
Currently, a significant disparity exists regarding the implementation of video-assisted thoracoscopic surgery (VATS) applied to anatomical lung resections at the population level.2,3 In our country, the most recent reference to the implementation of this surgical technique is included in the survey promoted by the Spanish Society of Thoracic Surgery (SECT).4
Despite the extensive literature concluding that VATS is associated with a lower rate of postoperative complications compared with open surgery, the conclusions concerning the effect of the approach on postoperative mortality are uncertain, with major meta-analyses and published population series showing no differences.5 On the other hand, traditional postoperative mortality (in-hospital mortality and/or 30-day mortality) only partially reflect the true surgical risk, which is best represented by the 90-day mortality rate.6
The GEVATS project was primarily designed to determine the effect of the eponymous surgery on the 90-day postoperative mortality rate following anatomical lung resection. Its secondary objective was to determine whether VATS influences the long-term oncological prognosis of patients who undergo surgery for lung cancer.
In this paper, we present the current practice of VATS in Spain and our initial results regarding the perioperative course after anatomical lung resection. Moreover, we describe the structure, methodology, and quality systems implemented by the GEVATS as well as the possible implications derived from the selection of patients, regardless of intention, of a voluntary multicentre study.
MethodsSpanish group of video-assisted thoracic surgeryThe GEVATS project of the Spanish Society of Thoracic Surgery (SECT) was founded in May 2015, and all thoracic surgery services of the Spanish National Health System were invited to become members. The research project was approved by the ethics committees of all the participating centres, and informed consent was obtained from the recruited patients to use their clinical data for scientific purposes.
A prospective multicentre cohort study was designed to record all anatomical lung resections performed within each participating department over 15 months (12/20/2016–03/20/2018). The oncological monitoring period ends on 03/20/2022.
Bilateral surgical procedures and those performed on patients younger than 18 years old were excluded.
At the beginning of the study, all the local researchers were informed that every centre would be audited after the recruitment had finished. However, the details of the audit to be undertaken were not intentionally announced.
DatabaseThe programming language used was PHP, under a Symfony development framework. The information was stored in a MySQL database that included 283 variables structured across the following five blocks: baseline characteristics, staging and pathological diagnosis, surgical procedure, postoperative morbimortality and oncological follow-up. Blocks 2 and 5 were relevant only for patients with lung carcinoma.
All variables were adapted based on the standardisation document of the Society of Thoracic Surgeons (STS) and the ESTS.7 Cases of postoperative morbidity included those occurring during the first 30 days or before discharge, and mortality was recorded at 90 days. Complications were classified based on whether they were respiratory, cardiovascular, or other according to the severity guidelines of the Clavien-Dindo classification.8
VATS was defined by consensus as the absence of rib spreading, regardless of the number of incisions performed. The interested reader can find online more detailed information about the database variables (supplementary material).
Sample sizeThe necessary sample size was calculated based on the primary objective of the study (i.e., to demonstrate differences in the 90-day mortality rate based on the type of surgical approach). As such, an independent proportionality analysis was performed using a chi-square test to estimate a mortality of 4% for open surgery (control group) and a mortality of 2% for VATS, with a VATS/open ratio of 1:3, an alpha level of 0.05, a statistical power of 0.8, and a two-tailed hypothesis test. The resulting sample size was 3238 patients (VATS, n=804; open, n=2434).
Auditing systemsIn addition to the filters in the database itself that served as a quality control during data entry by excluding implausible values and incompatibility between two or more variables, the following monitoring systems were established.
- 1)
Records with missing values regarding the key variables: “type of lung resection”, “type of surgical approach”, and “patient discharge status” were excluded.
- 2)
The recruitment rate of each centre, defined as the percentage of patients registered over all eligible patients (100×registered patients/eligible patients), was validated. To accomplish this goal, the local researcher of each department provided the GEVATS coordinator (RE) with an official document issued by the head of the clinical documentation department of the corresponding hospital indicating the number of lobectomies and pneumonectomies performed during the period of interest (20/12/2016–20/03/2018) using the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10).
Because this classification system co-codes atypical resections and anatomical segmentectomies, the latter were not specifically monitored. However, since the ICD-10 codes for lobectomy and pneumonectomy consider whether the surgical approach is endoscopic or open, the recruitment rate validation would allow us to obtain official data on the implementation of VATS.
- 3)
Centres that recruited fewer than 15 patients or had recruitment rates lower than 10% were excluded.
- 4)
For data validation purposes, we considered representative to audit a 20% sample of patients included by each centre (up to a maximum of 20 patients). This criterion involved the monitoring of 535 patients (i.e., 15.1% of the entire sample). The variables audited included the “date of surgery”, “type of lung resection”, “type of surgical approach”, “length of postoperative stay”, “occurrence of postoperative Grade IIIb-V complications” (respiratory, cardiovascular, or other), and “patient discharge status”.
The coordinator and internal scientific committee validated the data. To that end, each local investigator sent their corresponding hospital discharge reports based on a randomised list of recruited patients. Each patient to be audited was identified by the name of the .pdf file of their respective discharge report, which was equivalent to the GEVATS patient code. All other identifying information in the discharge report itself was hidden before being sent to the assigned auditor.
When necessary, the auditor requested additional and necessary clinical reports to certify the validity of the data (e.g., surgical protocol, intensive care unit report, and so on).
The similarity between the data recorded in the GEVATS database and those in the official documents was analysed for each department and for each variable audited. Accuracy was expressed as intervals, with an upper accuracy limit (100×matching data/verifiable data) and lower accuracy limit (100×matching data/all evaluated data).
Statistical analysisThe descriptive analysis of the data was performed using percentages for the qualitative variables and measures of central tendency (mean or median) and dispersion (standard deviation or 25–75th percentiles) were used for the quantitative variables depending on data distribution. Data normality was evaluated using the Shapiro–Wilk test and visual interpretations of the corresponding histograms.
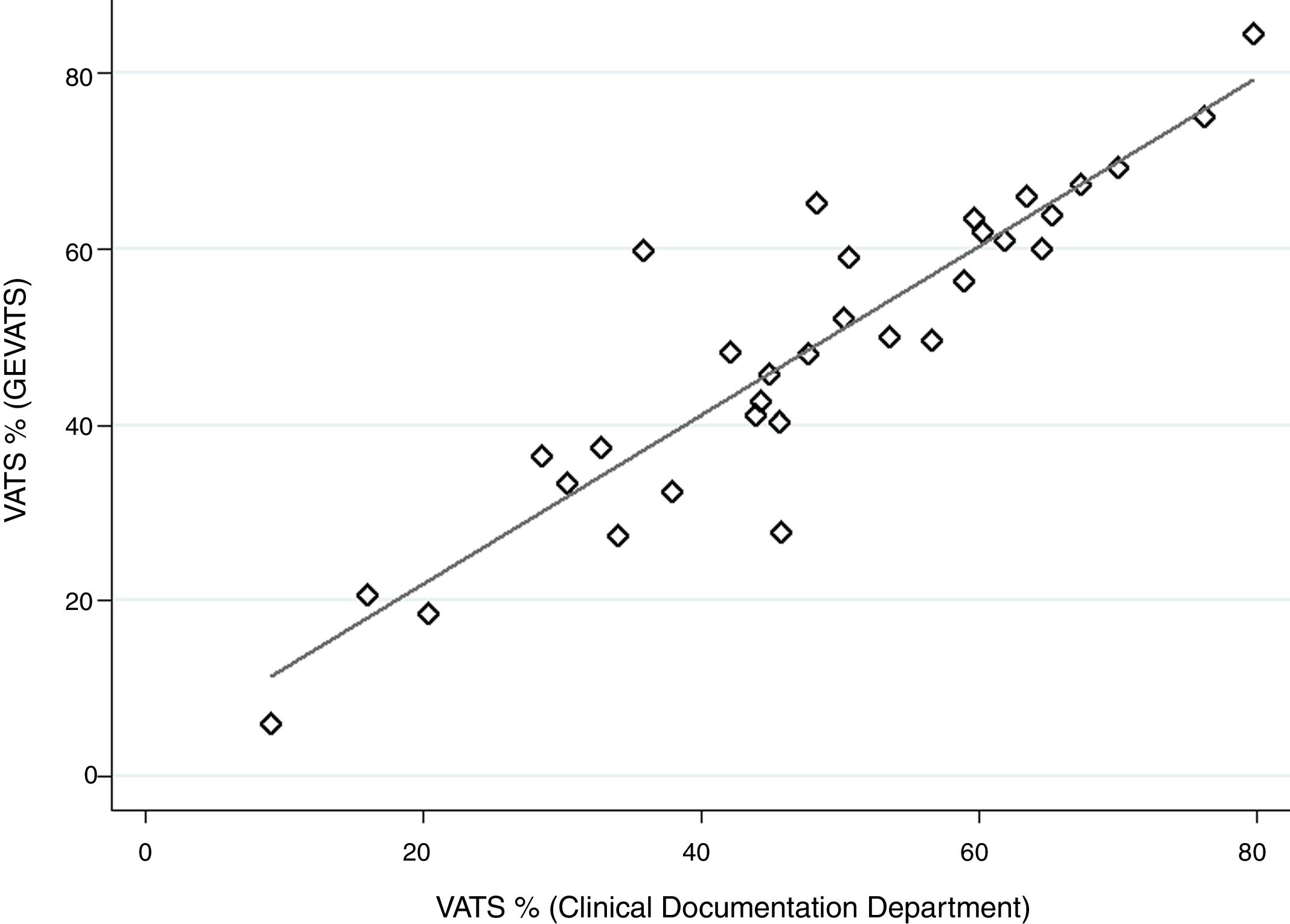
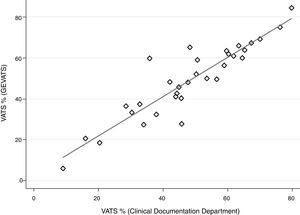
The correlation between the VATS percentages obtained from the administrative reports and the corresponding percentages recorded in the GEVATS database for each hospital were evaluated using Pearson's correlation coefficient (r) and represented by a scatterplot.
The 33 participating departments were grouped based on their recruitment rate: <80%, 80–94%, or 95–100%. The possible effect of low recruitment on the major postoperative variables (i.e., Grade IIIb-V complications during the first 30 days or before discharge and the 90-day mortality rate) was assessed using unadjusted and adjusted binary logistic regressions for age, sex, type of resection, predictive postoperative forced expiratory volume (FEV1ppo), and type of surgical approach. The results were expressed as odds ratios (ORs) with their respective 95% confidence intervals (95% CIs) and significance levels (p), using the group of hospitals with a recruitment rate of 95–100% as the reference. All data analyses were performed using Stata/MP 14.0.
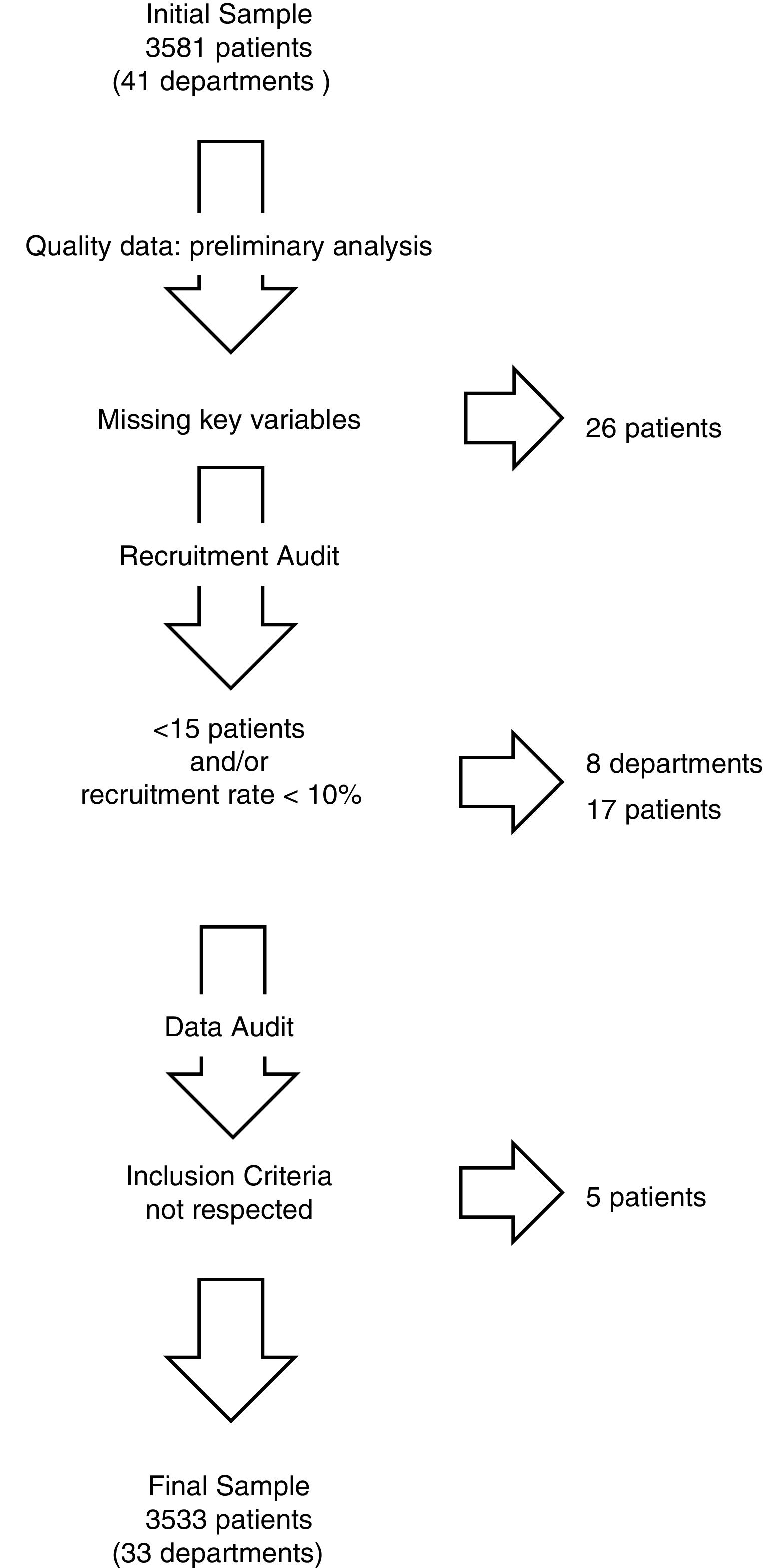
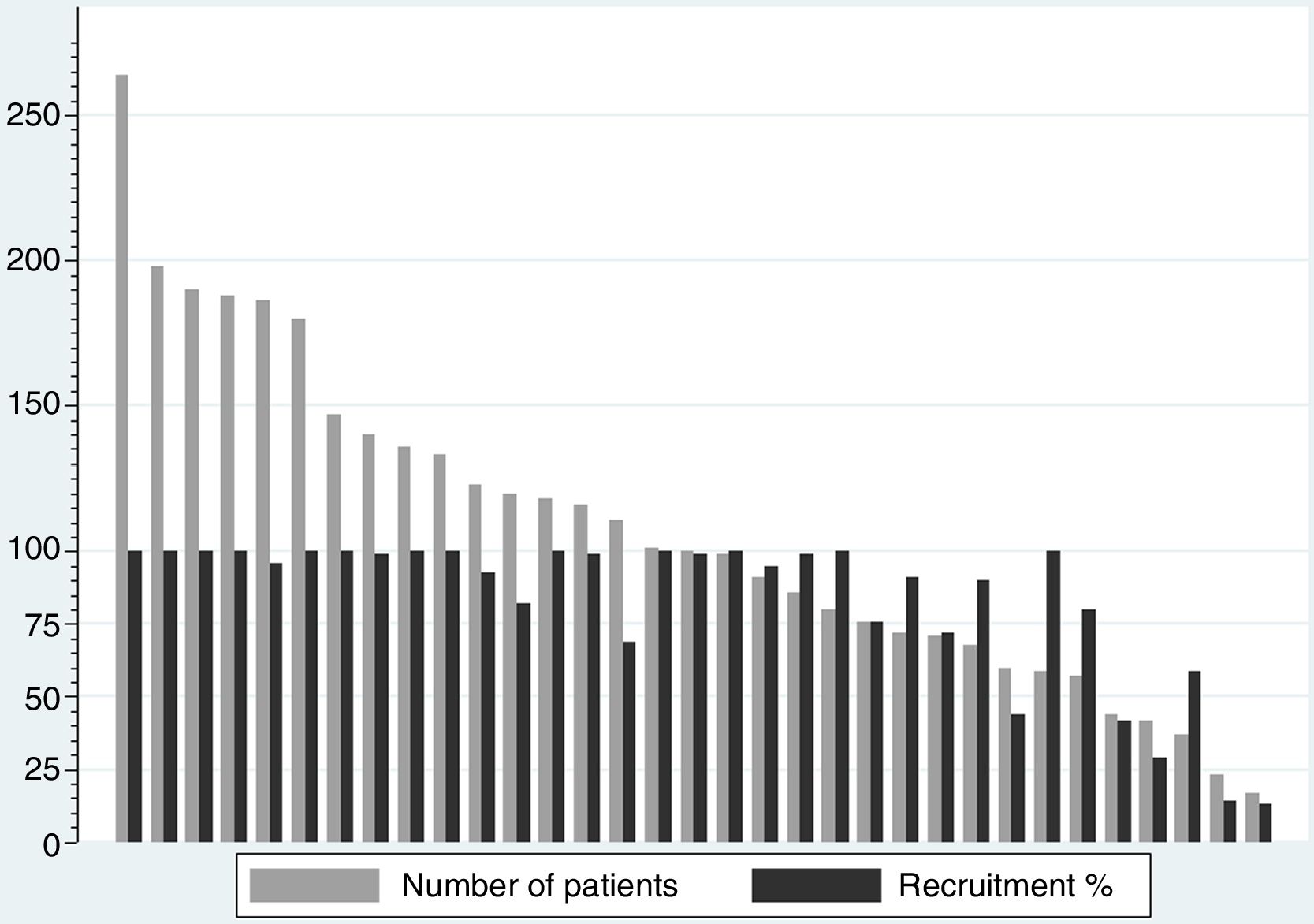
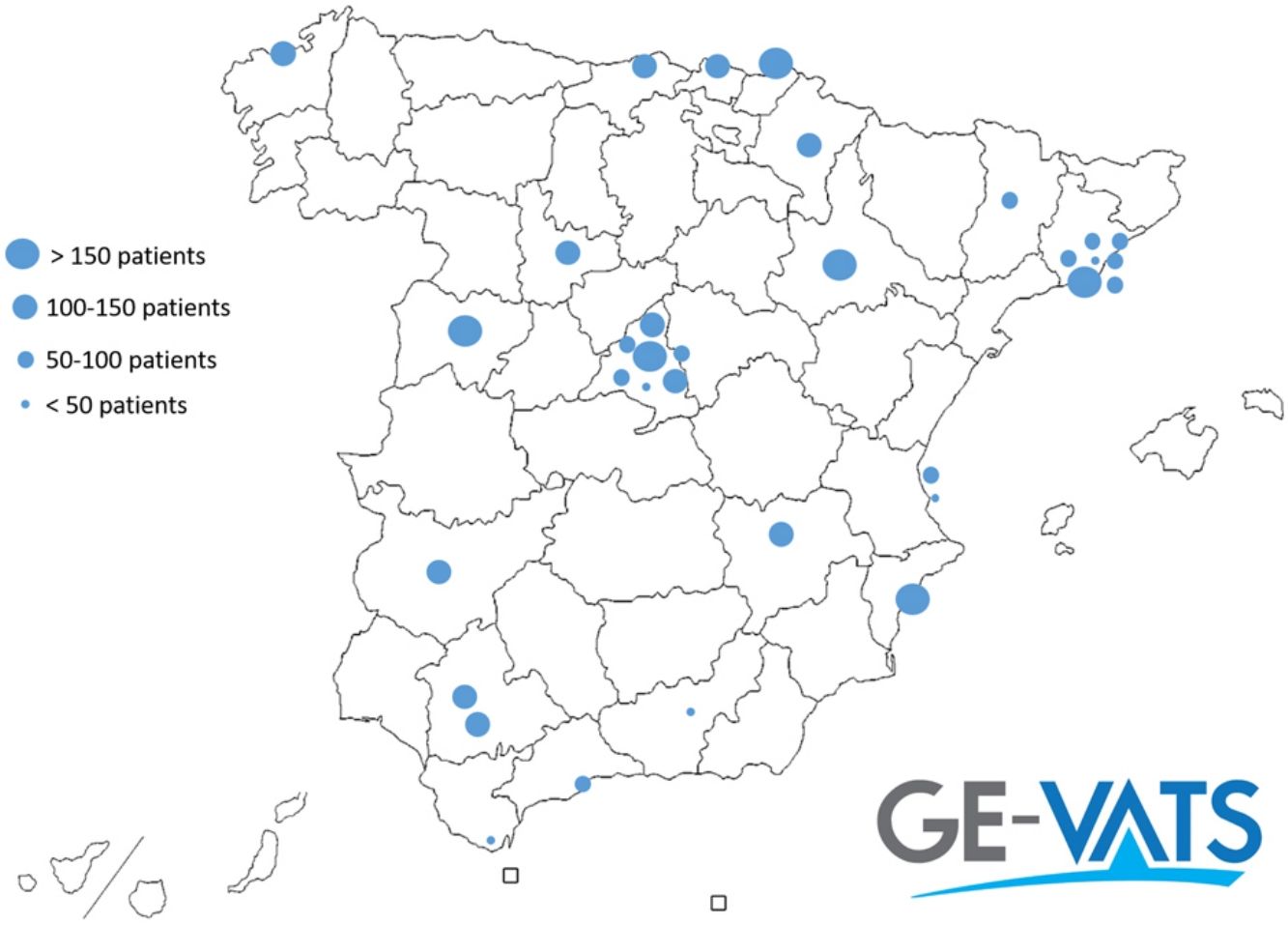
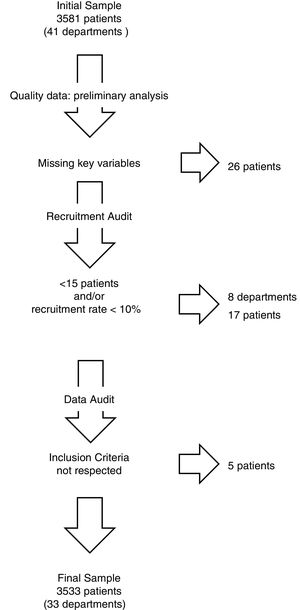
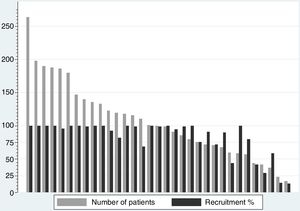
ResultsThe patients recruited and excluded because of the auditing systems are represented in a flowchart (Fig. 1). The number of patients included per hospital ranged from 17 to 264 (mean=107, standard deviation=57.2), with a median recruitment rate of 99% (25–75th percentile interval: 76–100%) and an overall recruitment rate of 83.3% (Fig. 2). Of the 33 departments, 13 reached 100% recruitment (1893 patients; 53.6% of the sample), six were between 95% and 99% (719 patients; 20.4%), five were between 80% and 94% (440 patients; 12.4%), and nine did not reach 80% recruitment (481 patients, 13.6%).
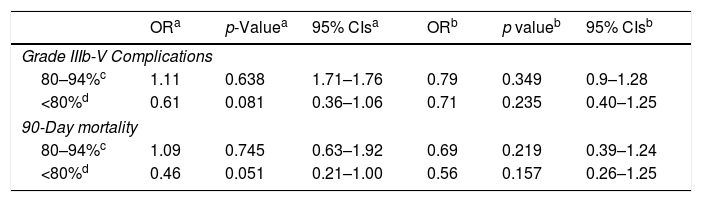
The analysis of the recruitment rate and its association with the presence of severe (Grade IIIb-V) postoperative complications and the 90-day mortality rate, using the group of hospitals with a recruitment rate ≥95% as the reference, was not significant. However, the unadjusted regressions revealed that a recruitment rate<80% was associated with a tendency to lower postoperative morbidity and 90-day mortality rates (Table 1).
Risks of major postoperative complications and mortality (30 days or before discharge) and the 90-day mortality based on the recruitment rate (19 departments with a 95–100% recruitment rate were used as the reference group; n=2612 patients).
| ORa | p-Valuea | 95% CIsa | ORb | p valueb | 95% CIsb | |
|---|---|---|---|---|---|---|
| Grade IIIb-V Complications | ||||||
| 80–94%c | 1.11 | 0.638 | 1.71–1.76 | 0.79 | 0.349 | 0.9–1.28 |
| <80%d | 0.61 | 0.081 | 0.36–1.06 | 0.71 | 0.235 | 0.40–1.25 |
| 90-Day mortality | ||||||
| 80–94%c | 1.09 | 0.745 | 0.63–1.92 | 0.69 | 0.219 | 0.39–1.24 |
| <80%d | 0.46 | 0.051 | 0.21–1.00 | 0.56 | 0.157 | 0.26–1.25 |
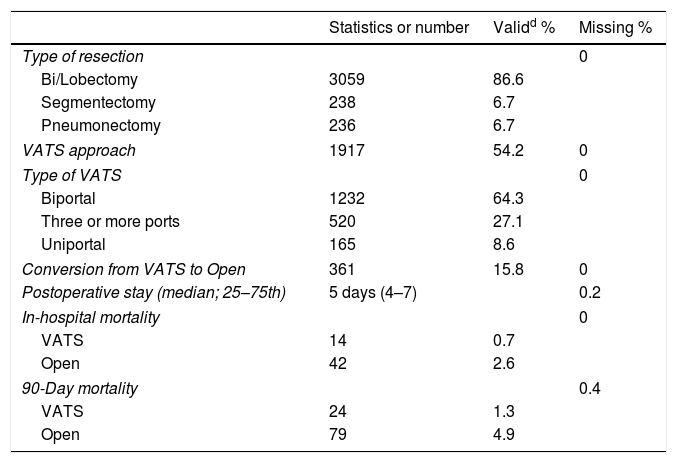
The overall percentage of procedures registered as VATS was 54.3% (1917/3533 patients), with a specific VATS rates for segmentectomy and lobectomy of 65.6% (156/238 pacientes) and 57.4% (1755/3059 patients), respectively. The percentages of VATS recorded by each hospital in the GEVATS database were highly correlated with the corresponding percentages based on administrative department reports, r=0.91 (Fig. 3).
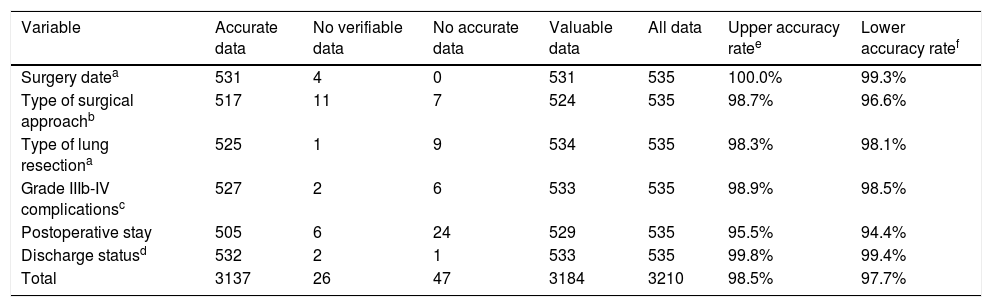
The overall accuracy percentage regarding the data recorded and the data evaluated based on the clinical reports of hospital discharge was excellent, ranging between 97.7% and 98.5% (Table 2).
Assessment of data accuracy base on six key variables or group of variables.
| Variable | Accurate data | No verifiable data | No accurate data | Valuable data | All data | Upper accuracy ratee | Lower accuracy ratef |
|---|---|---|---|---|---|---|---|
| Surgery datea | 531 | 4 | 0 | 531 | 535 | 100.0% | 99.3% |
| Type of surgical approachb | 517 | 11 | 7 | 524 | 535 | 98.7% | 96.6% |
| Type of lung resectiona | 525 | 1 | 9 | 534 | 535 | 98.3% | 98.1% |
| Grade IIIb-IV complicationsc | 527 | 2 | 6 | 533 | 535 | 98.9% | 98.5% |
| Postoperative stay | 505 | 6 | 24 | 529 | 535 | 95.5% | 94.4% |
| Discharge statusd | 532 | 2 | 1 | 533 | 535 | 99.8% | 99.4% |
| Total | 3137 | 26 | 47 | 3184 | 3210 | 98.5% | 97.7% |
The descriptive analyses of the major baseline, surgical, and postoperative variables, including data quality regarding missing values, are shown in table format (Table 3).
Description of the major variables included in the GEVATS.
| Statistics or number | Validd % | Missing % | |
|---|---|---|---|
| Type of resection | 0 | ||
| Bi/Lobectomy | 3059 | 86.6 | |
| Segmentectomy | 238 | 6.7 | |
| Pneumonectomy | 236 | 6.7 | |
| VATS approach | 1917 | 54.2 | 0 |
| Type of VATS | 0 | ||
| Biportal | 1232 | 64.3 | |
| Three or more ports | 520 | 27.1 | |
| Uniportal | 165 | 8.6 | |
| Conversion from VATS to Open | 361 | 15.8 | 0 |
| Postoperative stay (median; 25–75th) | 5 days (4–7) | 0.2 | |
| In-hospital mortality | 0 | ||
| VATS | 14 | 0.7 | |
| Open | 42 | 2.6 | |
| 90-Day mortality | 0.4 | ||
| VATS | 24 | 1.3 | |
| Open | 79 | 4.9 | |
The interested reader can find online more detailed information about the database descriptive analysis (supplementary material).
DiscussionThe Spanish VATS Group managed to recruit 3533 anatomical lung resections from 33 thoracic surgery departments in fifteen months (December 2016–March 2018). The audit process demonstrated an 83% overall recruitment rate and a 98% data accuracy across all departments. In addition, the data registered showed a 54% VATS rate (65.6% for segmentectomy and 57.4% in case of lobectomy).
Currently, the most commonly accepted quality standards related to the major indicators of the process and outcome of lung resection surgery are derived from the STS and ESTS databases. Recognising the immense potential of these projects to serve as a continuous source of knowledge for our specialty, the representativeness of the US and Europe is challenging. In fact, according to a recent report, the STS database only presented 25% centre and 38% patient penetrance by 2013.9
On the other hand, the representativeness of administrative databases is overshadowed by their deficiencies regarding the analysis of certain indicators, given the lack of specific clinical variables associated with a particular pathology or procedure.10
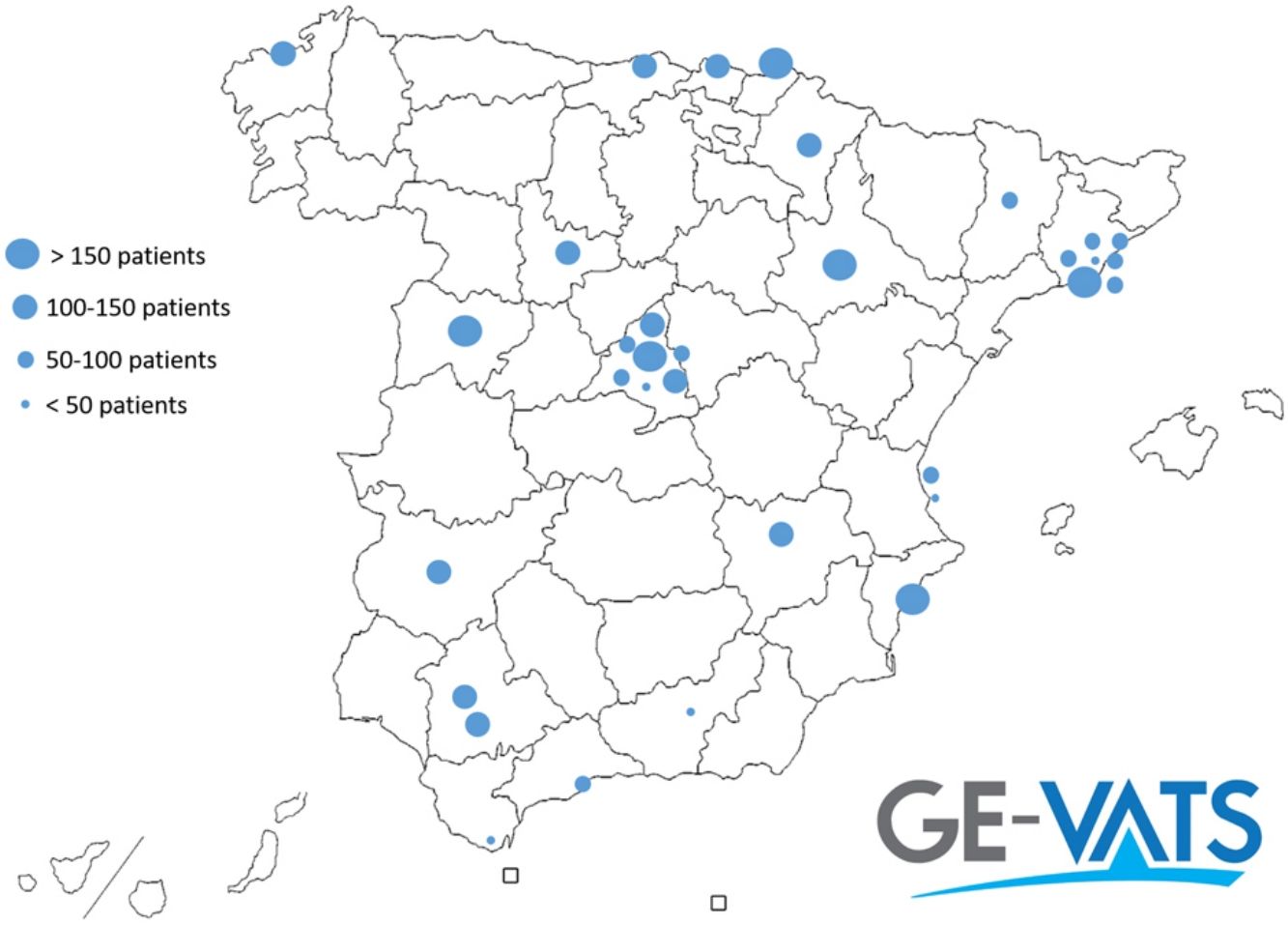
Spain, a country with a predominant National Health System, has 53 public departments of thoracic surgery. Of these departments, 33 (62%) are members of the GEVATS project. Regarding the representation of the Spanish territory, 12 out of 17 Autonomous Communities (71%) and 19 out of 30 (63%) Provinces with at least one thoracic surgery department are represented in our Group.
According to a report by the Spanish Ministry of Health, 30% of hospital discharges in 2018 derived from the private health system. However, only 9–10% of major thoracic surgical procedures (code 120 Diagnosis-Related Group) were performed out of a public institution throughout 2016 to 2017.11 Given that the overall recruitment of the GEVATS project was 83%, we could conclude that our sample included, approximately, 50%of the anatomical lung resections performed in our country during the study period.
Since the Spanish multicentre cooperative group dealing with videothoracoscopy for minor procedures (1573 patients, registered from 1996 to 1998), different nationwide surgical cohort studies and benchmarking projects have been developed in our country.12–16
Recently, the results of the Spanish multicentre prospective cohort study of the Group of Postoperative Complications of the Spanish Society of Thoracic Surgeons (GPC-SECT), has published the first known results about VATS implementation in Spain for lung cancer. This study registered 3307 patients operated on for lung cancer in 24 national thoracic surgery departments between June 2012 and November 2014. The percentages of VATS were 30.4% in men and 34.3% in women (9.3% of patients in that study underwent wedge resection), which means that the VATS implantation in our country, has nearly doubled after 5 years.17
One of the major handicaps of any voluntary database is the potential bias related to selection of patients to be included. In this sense, few studies have attempted to analyse and demonstrate this selection using administrative data or other mandatory population registers as a reference. In addition, studies that have attempted to demonstrate how this selection might influence the results and conclusions of a multicentric, national, and/or continental registry or database are rare.18 In our study, although we did not find a significant association between a lower recruitment rate and a lower complication rate, a trend was clearly present in the unadjusted analysis. The reasons for participating centres to optimise recruitment were not required but both, the loss of interest in the study and the necessary effort for data entry, could play definitive roles.
The estimates for sample size were only partially successful, since the percentage of VATS registered (54%) was notably higher than the expected value (25%). However, the estimated and registered values of 90-day mortality rates for VATS (registered vs estimated 2%) and open surgery (registered 4.9% vs estimated 4%) were somehow similar. This way, the recalculated sample size, based on the registered data, would have result in a sample of 718 patients (VATS 389 and Open 329 patients). Therefore, we can conclude that the GEVATS cohort will even allow stratified and propensity score analyses with enough statistical power as to obtain robust conclusions. The opportunity of clinical analyses based only on those centres with a 100% recruitment rate (1893 patients; 53.6% of the sample), could be another interesting chance for future projects related to the GEVATS cohort.
Although the validation of recorded data in multicentre registries is gaining popularity over the last years, the proportion of centres and patients audited is consistently low.19–21 In this regard, the recruitment rate of all the GEVATS departments and a stratified random sample of our cohort (15% of patients) were audited, including the most clinically significant variables or those considered as potential sources of conflict of interest. Agreement rate between our registered and official data were consistently high throughout the six key variables audited, in consonance with the results obtain by the STS database audits.22
The proportion of missing values is another known quality parameter of a database.23 Regarding the 242 variables comprising the four blocks analysed (baseline characteristics, diagnosis and staging, surgery, and postoperative period), the percentage of missing values was 0.95%. This value is excellent in terms of completion and perhaps the result of the design and filters implemented in the database, both of which were key during data entry.
Regarding our clinical results, the VATS lobectomy rate of 57.4% is worth mentioning because it is more consistent with the data published by the major North American databases than with the results derived from the European registry.2,3,24 Rates in excess of 50% in Europe have been published by the Dutch National Registry of Lung Surgery.25 Our in-hospital mortality rate (1.6%) and 90-day mortality rate (2.9%) are in line with or even lower than those published in other national studies.26
LimitationsGiven the voluntary nature of GEVATS and its manifest interest in minimally invasive surgery, one of our major limitations is related to the representativeness of the practice of VATS in Spain. Although 90% of the thoracic surgery departments in Spain have some degree of experience in performing anatomical lung resections via VATS (national survey, 2015), the actual figures might differ from those reported in this study.4
On the other hand, the auditing systems, excluding the reports issued by the departments of clinical documentation, were implemented by some of the member thoracic surgeons of GEVATS (the coordinator and the internal scientific committee) and not by a professional external auditing service, which might have influenced the reliability of our results. However, because one of the criteria to be audited was the degree of severity of postoperative complications, we emphasise the importance of the experience of the clinical professional in this regard.
ConclusionsThe GEVATS cohort represents, to date, the most ambitious prospective study of the Spanish thoracic surgery, regarding the number of centres involved, the total sample size, and the auditing systems implemented. Our results suggest that VATS is widely implemented in Spain.
Although our series did not demonstrate a significant association (only a trend between lower postoperative complications and lower recruitment rates), we believe that this parameter and its possible implications should deserve further attention by the main ongoing and future voluntary registries and multicentre studies of surgical series.
Last, the significant representativeness and excellent quality of our data will allow us to obtain highly reliable results in future projects, in which the effect of the surgical technique will be one of our primary foci.
Funding statementAll costs related to the start-up and maintenance of the GEVATS database were covered by Ethicon, Johnson & Johnson. The authors had freedom of investigation and full control of the design of the study, methods used, outcome parameters and results, data analysis, and production of the written report.
The GEVATS was awarded a grant from the Spanish Society of Thoracic Surgery as the best national research project of 2015.
Conflict of interestThe authors declare no conflict of interest.
We thank Johnson & Johnson for their collaboration in the development of the Spanish VATS Group. We also thank all those responsible for the clinical documentation services of each hospital for actively participating in the audit of our study.