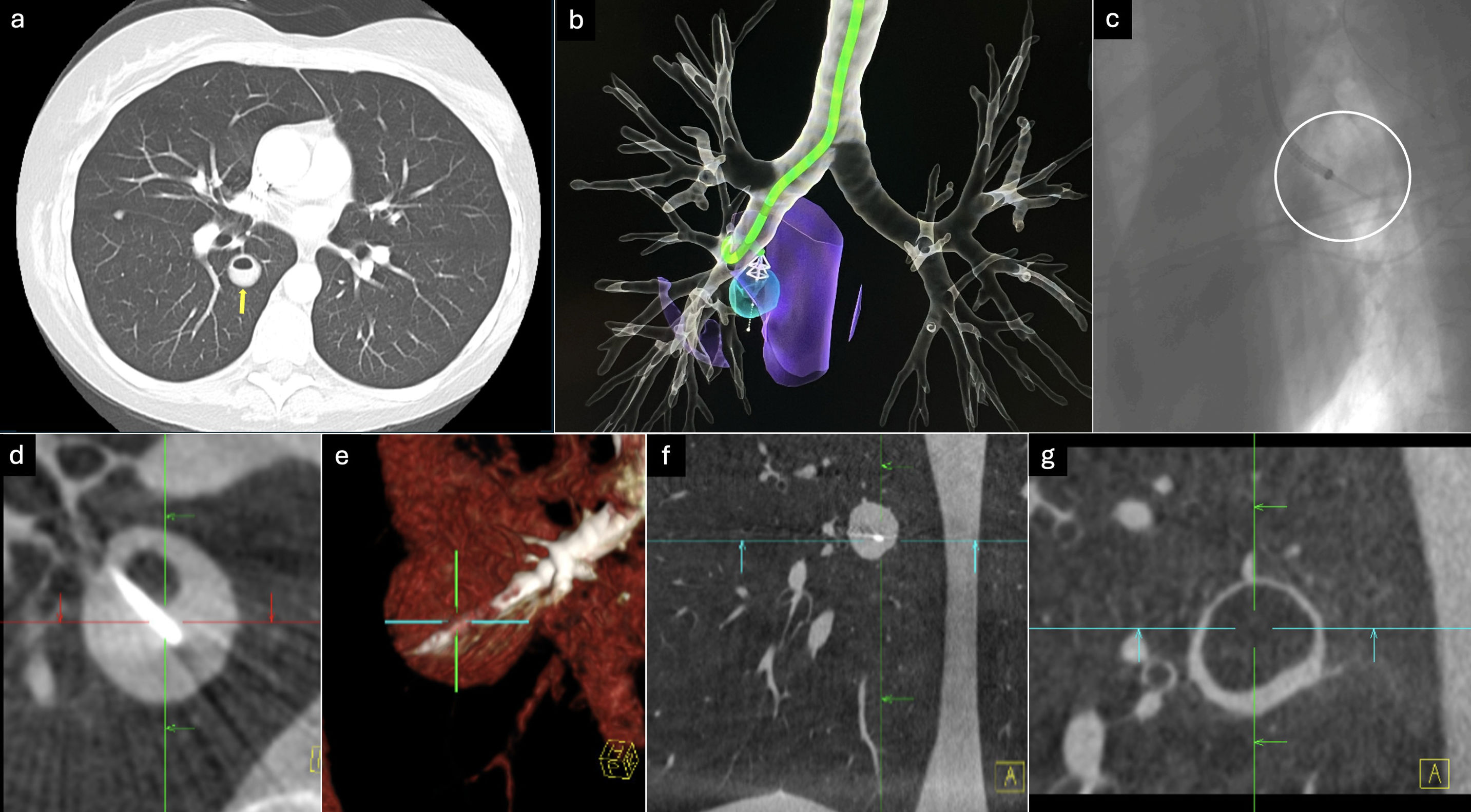
33-Year-old woman with a history of mixed connective tissue disease on immunosuppression with corticosteroids presented with abnormal CT chest showing a right lower lobe cavitated nodule of 19.8mm×19.6mm with airfluid level and no obvious bronchus sign. She underwent shape sensing Robotic-Assisted Bronchoscopy (ss-RAB) (Ion Endoluminal System, Intuitive Surgical, Sunnyvale, CA, USA) under general anesthesia and orotracheal intubation. Upon successful robotic navigation mobile cone beam CT (m-CBCT) (Cios Spin, Siemens Healthcare, Erlangen, Germany) was used to mitigate CT body divergence and secure optimal targeting of the lesion. A 3mm gap to the target was reached and a transbronchial puncture was performed with a 19G needle (Intuitive Surgical, Sunnyvale, CA, USA). A subsequent mCBCT spin (during inspiratory hold) secured successful tool in lesion. Approximately 3cc of purulent secretions were aspirated. Subsequent m-CBCT demonstrated successful drainage of the suspected lung abscess (Fig. 1). The microbiological result was compatible with Norcardia, and coverage with trimethoprim/sulfamethoxazole was started with good subsequent evolution. The ssRAB-mCBCT has revolutionized the diagnosis of difficult to access peripheral pulmonary nodules and there is experience in approaching cavitated and cystic lesions,1,2 however, the use of ssRAB-mCBCT as a tool for early drainage of lung abscesses is uncommon. The ssRAB-mCBCT could be a useful alternative in difficult access lung abscesses, small, central, without afferent bronchus. In our case, drainage of the entire contents was achieved and the causative germ was also identified, allowing specific antibiotic treatment from the beginning.
(a) Axial CT scan, cavitated image with airfluid level in the right lower lobe (yellow arrow). (b) Navigation path of the robotic-assisted bronchoscopy to the target (light blue circular image). (c) 3D fluroscopy image during aspiration of the lesion contents, showing the end of the robotic bronchoscope and the 19G needle (white circle). (d) mCBCT, showing a cavitated lesion with a airfluid level with the needle inside it. (e) 3D reconstruction of the tool in lesion. (f) mCBCT frontal view, the lesion is observed with heterogeneous content in its interior and hyperdense image of the tool. (g) mCBCT after the drainage of the purulent content of the lesion.
Conceptualization: all authors.
Methodology: all authors.
Formal analysis: all authors.
Data curation: AJ Solis and D. Abia-Trujillo.
Software: AJ Solis and D. Abia-Trujillo.
Validation: all authors.
Research: all authors.
Writing-preparation of the original draft: Solis AJ.
Writing-revising and editing: all authors.
Approval of the final manuscript: all authors.
Informed ConsentInformed consent was obtained from the patient for the publication of his clinical data and the use of diagnostic images.
Artificial IntelligenceWe do not use artificial intelligence.
FundingWe did not receive any funding.
Conflict of InterestsNone declared.