Earth-based analogue missions simulate aspects of space missions in a controlled, low-risk, and cost-effective environment, crucial for astronaut preparation. Sleep is a fundamental aspect for astronauts due to its impact on health, performance, and alertness. Disrupted sleep can significantly affect mission success and safety, causing exhaustion, excessive daytime sleepiness, mood alterations, and impaired concentration.1–3 Long-term consequences of sleep disorders are also well-documented.4–7 Despite numerous studies, analogue missions often involve few participants and vary significantly in design and duration.8 The lack of women's representation reflects broader underrepresentation in space missions, with only 11% of astronauts and 7% of women having performed spacewalks (UNOOSA).
This observational prospective study was conducted in April 2023 during a 2-week simulation mission at the Mars Desert Research Station (MDRS), operated by The Mars Society in a remote location in southern Utah. The facility comprises an enclosed habitat, greenhouse, science dome, two telescopes, maintenance pod, and vehicles for simulated surface activities. Although MDRS cannot replicate Martian gravity, solar radiation, circadian rhythm or atmospheric composition, it accurately mimics social factors, isolation, Extra-Vehicular Activities (EVAs) protocols, conserving limited resources of food, water and energy, and structured communication with mission control.
The Hypatia I crew comprised 7 adult women from Catalonia, Spain (age: 36.86±7.67 yr; weight: 59.71±5.68kg; BMI: 21.03±1.66kg/m2) with diverse academic backgrounds. Informed consent was obtained and the Ethics Committee on Clinical Investigation of the Hospital Universitari Germans Trias i Pujol approved the study (code: PI-23-270).
Participants wore the Fitbit Sense 2 (Fitbit Inc, San Francisco, CA, USA by Google) smartwatch on their non-dominant wrist throughout designated 24-h periods, collecting data synced via the Fitbit app and stored on Fitbit services. Although Fitbit Sense 2 provides a great deal of data, we focused on the following key variables: sleep time, wake time (“WASO”, for wake after sleep onset) and rest time; REM, light and deep sleep duration; and number of awakenings. Additionally, participants maintained a daily self-reported sleep log noting sleep time, instances of daytime sleepiness and subjective sleep quality.
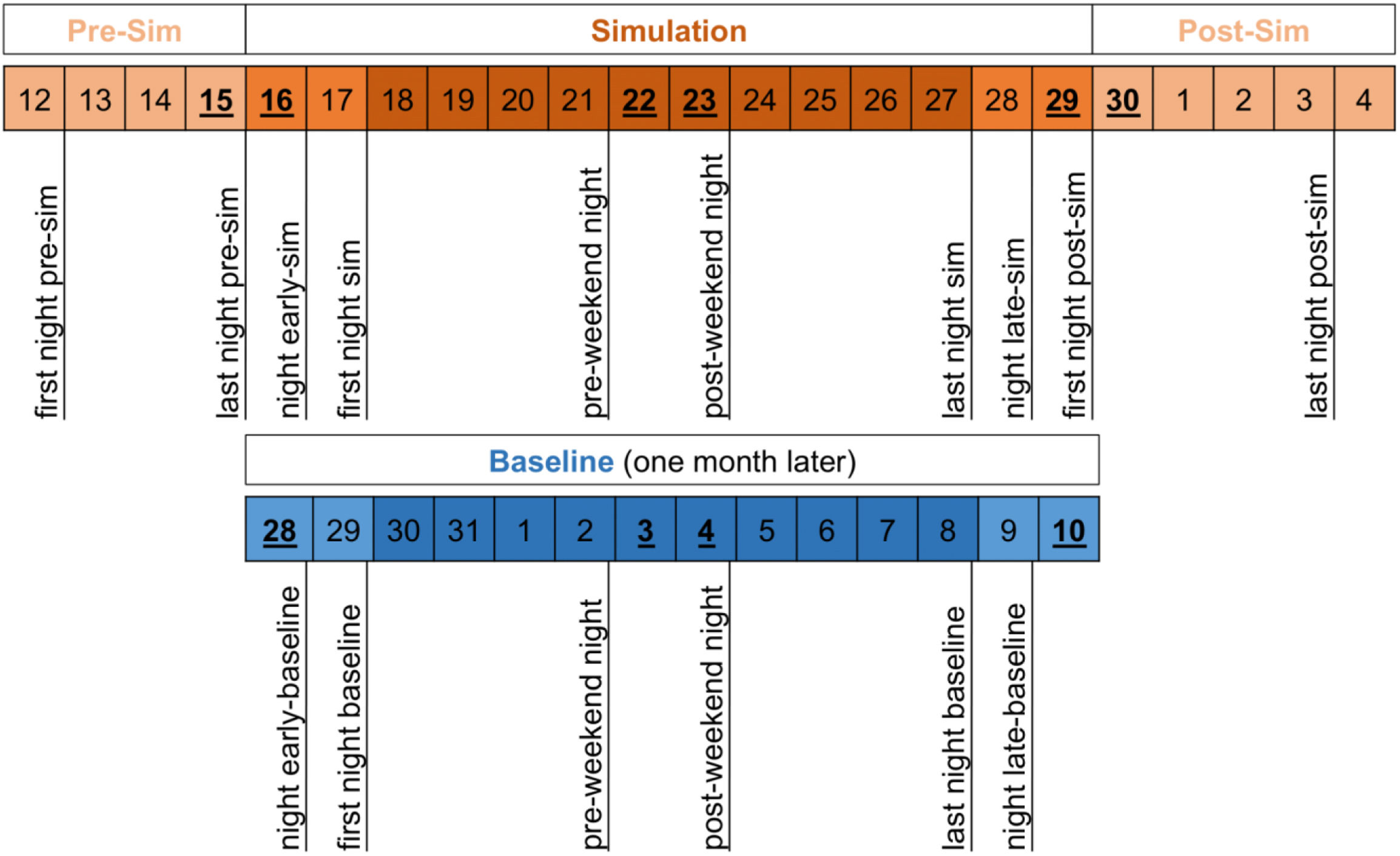
We defined two assessment periods: simulation and baseline, each of which divided to account for specific characteristics (Fig. 1). For instance, the first night pre-simulation considered jet lag effects. No sleep data were recorded on April 29–30, as most of the participants had early morning international flights home. Separate analyses were conducted for weekends, acknowledging potential variations in activity and routines. Due to extensive pre-mission preparations, the baseline period was measured one month after the mission to better reflect participants’ regular routines.
Sleep, WASO and rest time and REM, light and deep sleep time have been used for the intra and inter groups analysis. T-Student test for parametric samples and Wilcoxon test for non-parametric variables were used to determine statistically significant differences between groups (simulation and baseline) for each night. For the intra-groups analysis (comparison between nights of the same group), repeated measures analysis of variance (ANOVA) for normally distributed variables and Friedman test for non-normally distributed variables were used. Bonferroni correction was applied for multiple groups comparison.
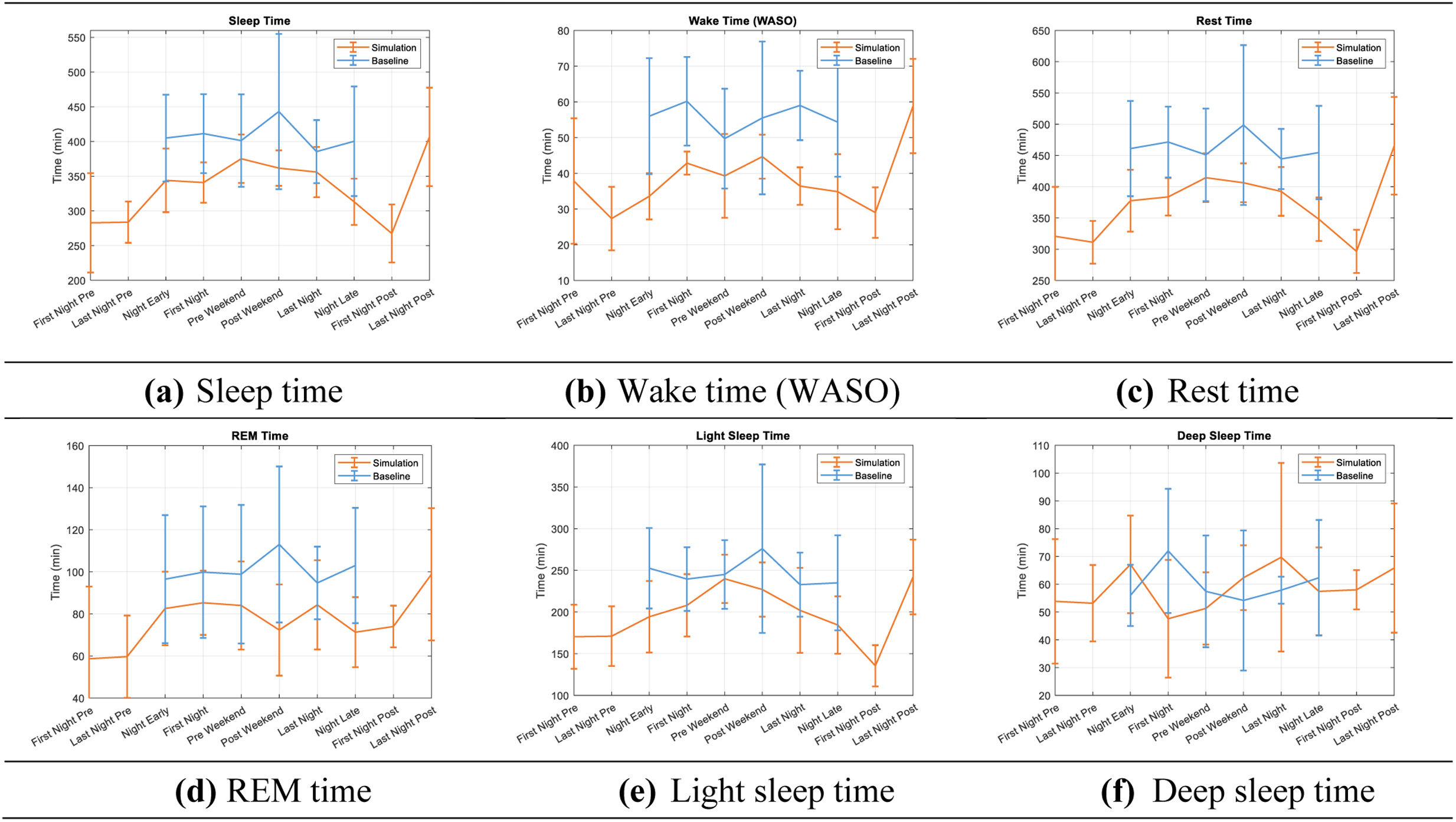
Fig. 2 shows the evolution in sleep time, WASO, rest time, REM time, light sleep time and deep sleep time parameters during simulation (orange) and baseline (blue) periods, with error bars representing standard deviation for each night. Intra-group differences (differences in sleep parameters between nights for both, simulation and baseline periods) were evaluated, revealing no significant differences during the baseline period. In simulation, significant differences were found in sleep time (first night sim vs. last night post-sim, P<0.01), WASO and rest time (last night pre-sim vs. last night post-sim, P<0.05 and P<0.01 respectively).
Significant differences were observed between simulation and baseline periods in various sleep parameters (Tables S1 and S2). Notably, participants experienced decreased REM sleep and less light sleep (P<0.05) in late night during simulation. The analysis of self-reported sleep logs reveals an average sleep quality rating of 7.2 during simulation and 7.1 at baseline.
Our investigation revealed differences in sleep quantity and quality during the simulation compared to baseline.
Participants experienced shorter sleep duration, reduced WASO, and overall decreased rest time during the analogue mission. These findings parallel those reported by Chen et al.9 in a study involving a three-member, all-male crew during a 15-day spaceflight; a temporal window comparable to our study. However, they contrast with the Mars-500 study,10 where participants showed increased lethargy and decreased movement during waking hours as the mission progressed; these trends were not evident during the first three months and the last 20 days of the mission. A closer analysis of our study data revealed an initial upward trend in sleep and rest duration during the first half of the mission, followed by a decline in the latter half. A more protracted study duration might yield results similar to those observed in the Mars-500 study. Despite shorter sleep, relative values found a sleep efficiency (89.94%) and a WASO (10.05%) within normal ranges. This finding suggests that participants adjust to a more efficient sleep pattern in response to their reduced sleep duration during the simulation.
Furthermore, our results revealed reduced REM sleep during simulation, but with an acceptable mean percentage of 22.71%. Self-reported sleep logs showed no significant differences in sleep quality between simulation and baseline periods. Sleep deprivation, particularly REM sleep reduction and circadian rhythms disturbances, can impair alertness and performance.11,12 In previous studies, astronauts report lower subjective rating of sleep quality during missions,11,13 difficulty falling asleep and frequent sleep interruptions while in orbit.14 In Flynn-Evans et al.’s study15 astronauts attributed these difficulties to the demanding workload. Diverse roles within the mission likely contributed to interpersonal sleep pattern differences and shows that subjective sleep quality not only depends on sleep duration and percentage of sleep phases, but also on various other factors.
Women respond differently to sleep disorders and deprivation compared to men, contributing to specific health outcomes.16,17 Although hormonal differences may influence, and menstrual cycle data was collected, the study's short duration did not allow for a complete cycle to be captured, so we decided not include this information.
While polysomnography remains the gold standard for sleep studies, it's impractical for real space missions. Fitbit sense 2 has proven successful for monitoring sleep and wakefulness,18 despite the known limitations of older models in accurately determining sleep stages, especially in individuals with health conditions. However, technology evolves rapidly, and recent versions have shown improvements,19 with high sensitivity and accuracy in determining sleep stages.
The Mars-500 study's findings on lethargy and reduced physical activity highlighted the importance of daily exercise routines in subsequent missions. However, despite conclusive scientific evidence demonstrating the relevance of sleep disturbances, concrete measures to enhance sleep in real space missions have not been implemented. Successful attempts to implement countermeasures were demonstrated in an experiment during the robotic Phoenix Mars Lander spacecraft, where mission personnel worked on a Mars day (24.65h) for 78 days.20
In conclusion, our study underscores the intricate relationship between sleep quantity, quality, individual differences, and mission demands in simulated space conditions and contributes to bridging the existing data gap on women's health in space.
We sincerely thank the Innovation Unit of the Hospital Universitari Germans Trias i Pujol for their invaluable support and collaboration throughout our research. Special gratitude goes to Google for providing the Fitbit Sense 2 devices, essential for data collection. We appreciate the Mars Society for allowing us to conduct our research at the Mars Desert Research Station. Our heartfelt thanks go to the Hypatia I crew for their voluntary participation and long-term commitment to scientific research with a gender perspective. We also acknowledge all individuals and institutions whose contributions were essential to the success of the Hypatia I mission, emphasizing that without their support, this project would not have been possible.
The Hypatia I analogue mission received support from the Catalunya La Pedrera Foundation, the Government of Catalonia, the Banco Sabadell Foundation, the Girls and Space Club, the Catalan Foundation for Research and Innovation, and isardSAT. The funding sources had no involvement in the preparation of this article, including the study design, data collection, analysis, and interpretation, writing of the report, and the decision to submit the article for publication.