In humans, hydatid disease is most frequently caused by Echinococcus granulosus. It is endemic in many countries where livestock is bred, and it is usually located in the liver (50%–75%) and lungs (15%–25%). Mediastinal presentation is very rare and represents 0.1%–0.5% of all locations.1 The case that we present is multiple mediastinal hydatidosis, quite probably secondary to hydatid dispersion from a previous intervention, which posed a surgical challenge given the multiplicity of the lesions.
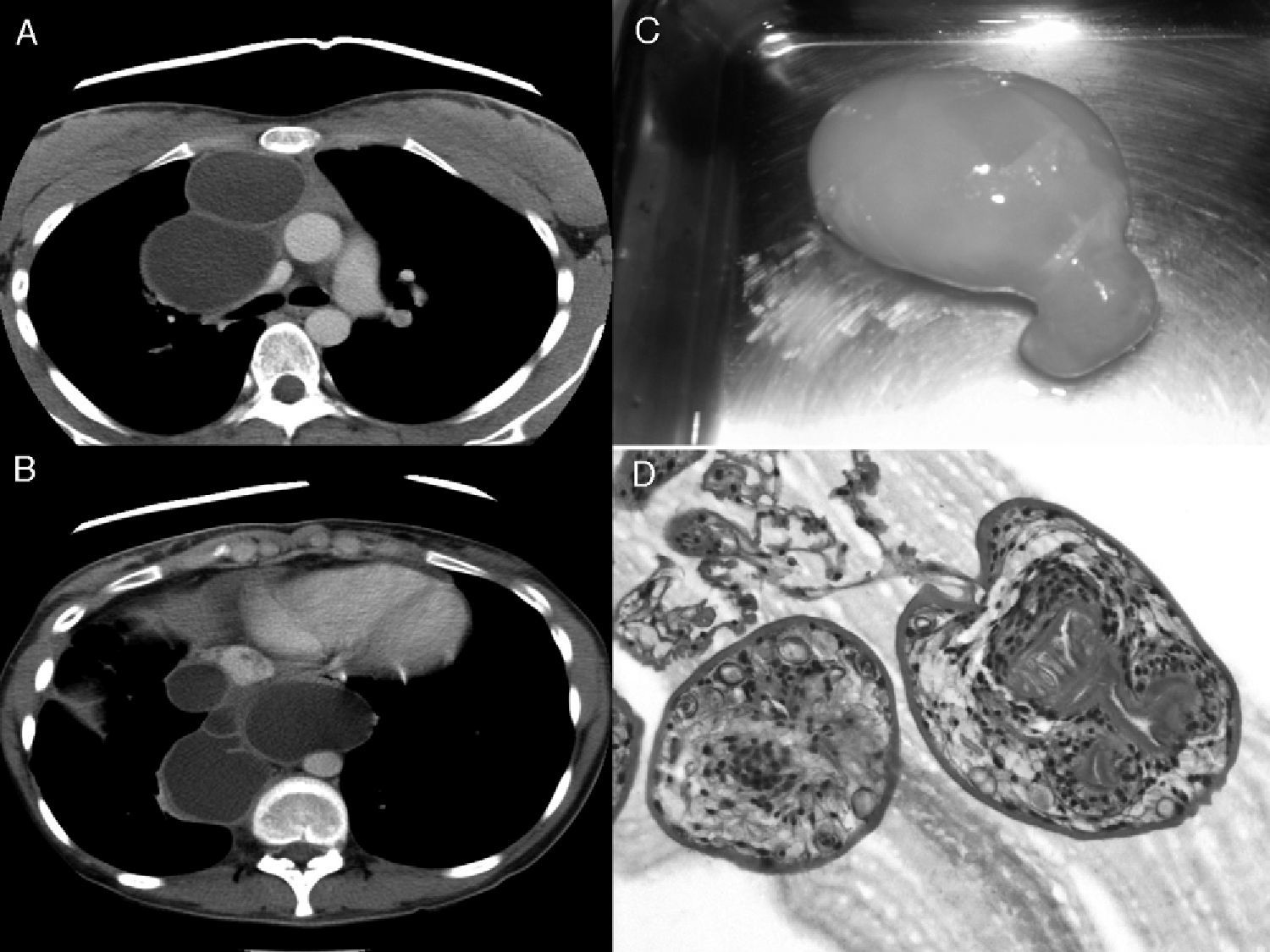
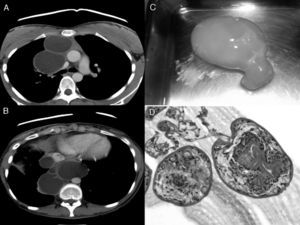
The patient is a 20-year-old woman, originally from Moldavia, who came to the emergency department in March 2011 complaining of sharp chest pain in the right anterior region that had been evolving over the course of the previous 2 months, along with mild dysphagia for both solids and liquids. Her medical history included the resection in Moldavia of a “lung parasite” by means of right thoracotomy in 2006, followed by one year of anti-parasitic treatment. Physical examination confirmed a scar from the right posterolateral thoracotomy and blood work showed mild anemia (Hb 11.7) with no leukocytosis or eosinophilia, with negative hydatid cyst serology. Imaging studies, including chest radiography, computed tomography (Fig. 1A and B) and magnetic resonance, revealed mediastinal widening due to the presence of multiple cystic mediastinal masses with affectation of the 3 compartments and craniocaudal extension, which produced a significant mass effect on the adjacent vascular structures and esophagus, with a minimal quantity of pericardial effusion. The liver presented no findings. Given the patient's history, we suspected mediastinal hydatidosis that was probably secondary, and right re-thoracotomy intervention was programmed. After the release of intense pleural adhesions, resection of the pericyst was initiated (Fig. 1C) with complete resection of all the cysts that had been observed by imaging techniques, using continuous lavage with hypertonic saline. The pericysts were resected, and those that could not be completely resected were left flat. The post-op period transpired without incident, and treatment was initiated with 400mg albendazole every 12h; the patient was released from the hospital after 7 days. Anatomic pathology and microbiology reports confirmed the presence of E. granulosus. With an optical microscope (Fig. 1D), the cystic capsule was able to be observed, which was made up of laminated membrane and germinal layer, with freed scolex. PCR detected nucleic acids of E. granulosus. To date (18 months later), there have been no symptoms or radiological signs of relapse.
(A and B) Computed tomography: axial slices obtained with mediastinal window showing a large multiseptated multicystic mass with linear enhancement extending in a craniocaudal direction. It affects the 3 mediastinal compartments and conditions the mass effect on adjacent vascular structures (superior cava in A and esophagus in B). (C) Entire hydatid obtained after opening the pericyst. (D) Image obtained by H–E 20× stain: hydatid cyst with laminated membrane and freed scolex; scolex with 4 suckers and rostellum with double crown of hooks.
Hydatid disease in humans is caused by the larval from of Echinococcus. Medically, the 2 most important species are E. granulosus and E. multilocularis, which cause cystic echinococcosis (CE) and alveolar echinococcosis, respectively.2 The annual incidence of CE is <1 to 200 cases per 100000 inhabitants in endemic areas like Eastern Europe and the Mediterranean, although cases are also seen in other countries. In primary CE, metacestodes (the larval form of the parasite) can develop in almost any organ. The most frequent locations of the disease are the liver (50%–75%) and the lungs (15%–25%), and intrathoracic extrapulmonary areas are rare. Cases have been described with mediastinal (most frequently posterior), pleural, pericardial and chest wall affectation.3 Secondary CE develops from the scolex disseminated by a fertile primary cyst, as may have occurred in our case given the history of previous lung hydatid surgery. After hydatid rupture, the probability of a secondary hydatidosis is approximately 10%, since the cysts are not fertile in 90% of episodes.3 Hydatid cysts located in the mediastinum can become large in size due to the low resistance offered by adjacent structures, and the symptoms depend on the size and the compression of proximal structures (dyspnea, retrosternal or chest pain, cough, dysphagia or upper vena cava syndrome), and complications can be fatal, such as perforation of vessels or bronchi, infection or anaphylactic shock.4 Once the diagnosis has been established and before said complications appear, surgical treatment is indicated; suspicion is based on clinical history, serology and radiology. Mediastinal hydatidosis is not distinguishable from other cystic lesions of the mediastinum, and the definitive diagnosis is not made until surgery. Although many serology tests have been proposed, they are not routinely done in most studies.5
Whenever possible, the treatment of choice is surgical resection of the cyst and adjacent pericyst tissue. When there are multiple mediastinal lesions, complete resection should also be attempted before any complications can be caused by the rupture of a cyst4,6 (pleural effusion, empyema, anaphylactic shock). If this is not possible because vital structures are affected, partial pericystectomy can be done before extirpation of the cyst. The surgery is associated with a recurrence rate of 1.5%–2.5%,5 and treatment with albendazole (10–15mg/kg/day) or mebendazole (40–50mg/kg/day) is also recommeded.2 We conclude that, even though secondary mediastinal hydatidosis remains a rare disease, when it does arise, surgery should be contemplated and complete resection should be attempted before any complications occur due to cyst rupture.
Please cite this cite as: de Olaiz Navarro B, et al. Hidatidosis mediastínica secundaria. Arch Bronconeumol. 2013;49:87–8.