Psoriasis is a chronic inflammatory disease mainly affecting the skin. The pathogenic mechanism of this condition is largely due to overstimulation of CD4 Th1 and Th17 lymphocytes, which have a well-established role in the formation of sarcoid granulomas.1
We present the case of a 38-year-old woman with a diagnosis of severe psoriasis vulgaris, with a finding of mediastinal lymphadenopathies and ground glass infiltrates, finally diagnosed as sarcoidosis.
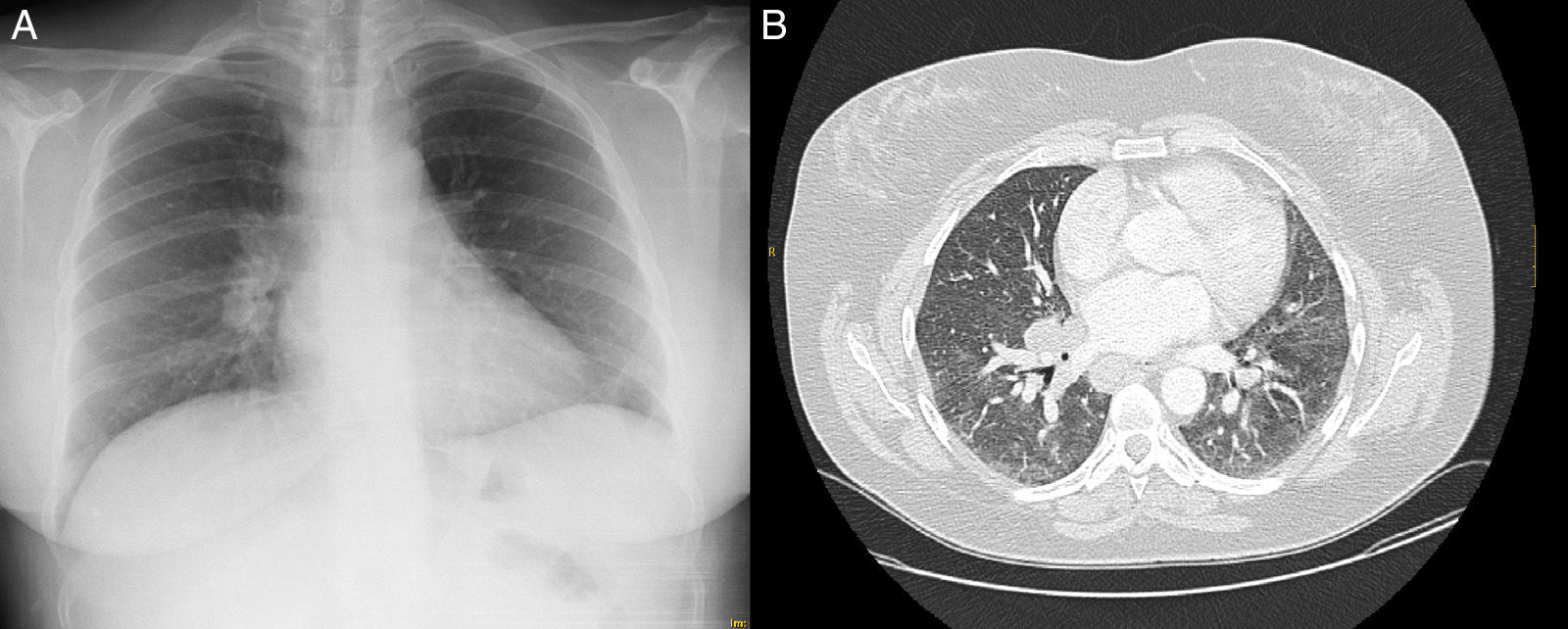
A 38-year-old woman with a 9-year history of severe psoriasis vulgaris (Fig. 1) receiving treatment with topical corticosteroids. A chest radiograph and Mantoux testing were performed before starting systemic biological therapy. She had no respiratory symptoms, but the radiograph showed a chance finding of right hilar lymphadenopathies (Fig. 2A). The examination was completed with a chest computed tomography (Fig. 2B), showing pathologically enlarged hilar and mediastinal lymph nodes and bilateral ground glass parenchymal infiltrates. Angiotensin-converting enzyme levels were normal. Fiberoptic bronchoscopy was performed. Bronchial aspirate and bronchoalveolar lavage (BAL) cultures were negative, and cytology was also negative for malignancy. BAL immunophenotyping revealed a lymphocyte population composed predominantly of CD3+ (96%) with a CD4/CD8 ratio of 6.67. Endoscopic ultrasound-guided fine-needle aspiration was performed, but the sample was poorly representative and the result was inconclusive. Mediastinal lymphadenopathy biopsy was performed using video-assisted mediastinoscopy, revealing blurred lymph node architecture occupied by multiple confluent granulomas of a similar size, formed of epithelioid-like histiocytes, with no necrosis and the presence of multinucleated giant cells. PAS and Ziehl-Neelsen stains were negative. All these findings were consistent with the diagnostic suspicion of stage II sarcoidosis.
Psoriasis is one of the most common systemic inflammatory diseases. It is characterized by increased immune system activity, mainly derived from activation of the Th1 and Th17 lymphocytes.
Sarcoidosis is a chronic disease characterized by the formation of non-caseifying epithelioid granulomas, most commonly in the lungs, skin and eyes. Although the etiology is still partly unknown, we know that the immunological basis of the disease consists of an accumulation of CD4 T cells in the inflammation sites, which interact with macrophages, causing an imbalance in favor of a Th1 cytokine profile, which finally triggers the granulomatous inflammatory process.1 The role of the Th17 lymphocytes in the formation of sarcoid granulomas has also been established, as has their importance in the alveolitis phase and in progression to the fibrotic stage of the disease.1
Very few cases of concomitant psoriasis and sarcoidosis have been reported,2–4 although recently a greater risk of presenting sarcoidosis has been observed in psoriasis patients compared to the general population, an association that moreover is severity-dependent.5
These data all go to support the hypothesis of a shared pathogenic pathway, although studies are needed to elucidate the possible role of other factors, such as the sarcoid disease phenotype, a possible paradoxical effect of treatment of the psoriasis itself (a phenomenon described with anti-TNFα antibodies6), the importance of environmental factors such as smoking, and the possible clinical, prognostic and therapeutic implications of the combination of both diseases.
Please cite this article as: Santalla Martínez M, Loureiro Martínez M. Asociación psoriasis-sarcoidosis: 2 entidades y una vía patogénica común. Arch Bronconeumol. 2016;52:489–490.