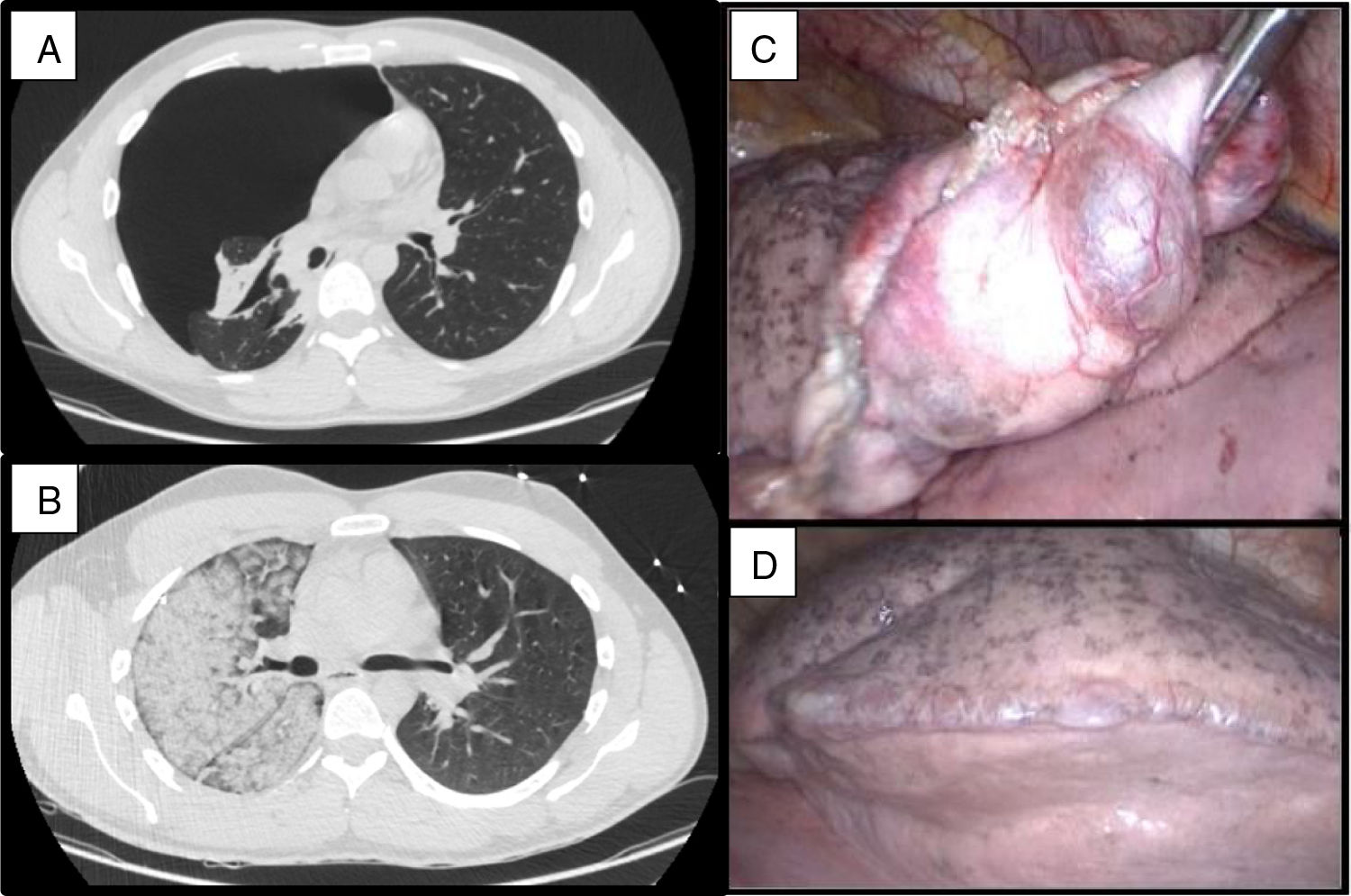
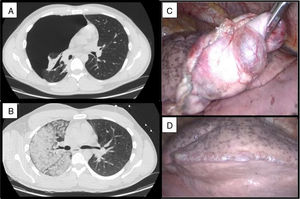
Our patient was a 28-year-old man, who, after a 5-day history of pleuritic pain, was diagnosed with complete right pneumothorax on chest CT. After insertion of a 10F pleural drainage tube connected to −20cm H2O suction the patient developed irritative cough, central chest pain, hypotension, tachycardia, and desaturation. He was stabilized in the ICU, and a repeat CT scan was requested, showing ground glass opacities in the right lung, consistent with reexpansion pulmonary edema (Fig. 1). The patient did not improve and required invasive mechanical ventilation. Extubation was achieved after 48h. Apical bullous lesions and multiple blebs were observed during surgery for bullectomy and mechanical pleurodesis by video-assisted thoracoscopy. The pleural drainage tube was removed and the patient was discharged 72h after surgery, without complications.
Reexpansion pulmonary edema, first described in 1853 by Pinault, is a rare complication, usually less than 1%, that occurs after rapid reinflation of the lung following evacuation of a pneumothorax or pleural effusion. Mortality can be as high as 20%.1 Diagnosis is clinical, supported by imaging tests. Treatment is based on supportive measures, requiring CPAP or even IMV with PEEP in the most severe cases, as occurred in our patient. Clinical suspicion is fundamental to guiding diligent action.2
Please cite this article as: Cózar Bernal F, Zúñiga Sánchez LG, Barrero García I. Edema de reexpansión pulmonar ¿mito o realidad? Arch Bronconeumol. 2021;57:492.