We present the case of a 60-year-old man with a history of active smoking (40packs/year), COPD, right upper lobe pneumonia and tubercular esophagocutaneous fistula. He worked as a sandblaster for 25 years and generally failed to use protection in the workplace.
Over the previous months, he had suffered progressive dyspnea with no cough, fever, expectoration or associated constitutional symptoms.
On auscultation, several disseminated rhonchi were found in both lung fields. No significant findings were revealed on general laboratory testing and venous blood gases were as follows: pH: 7.45; PCO2: 35; PO2: 92; SaO2: 97%. Lung function testing showed a mixed pattern with forced vital capacity (FVC) 2.67L (72%), forced expiratory volume in 1s (FEV1) 1.67L (57%), FEV1/FVC: 62% and forced expiratory flow between 25% and 75% of vital capacity (FEF: 25–75) 51%.
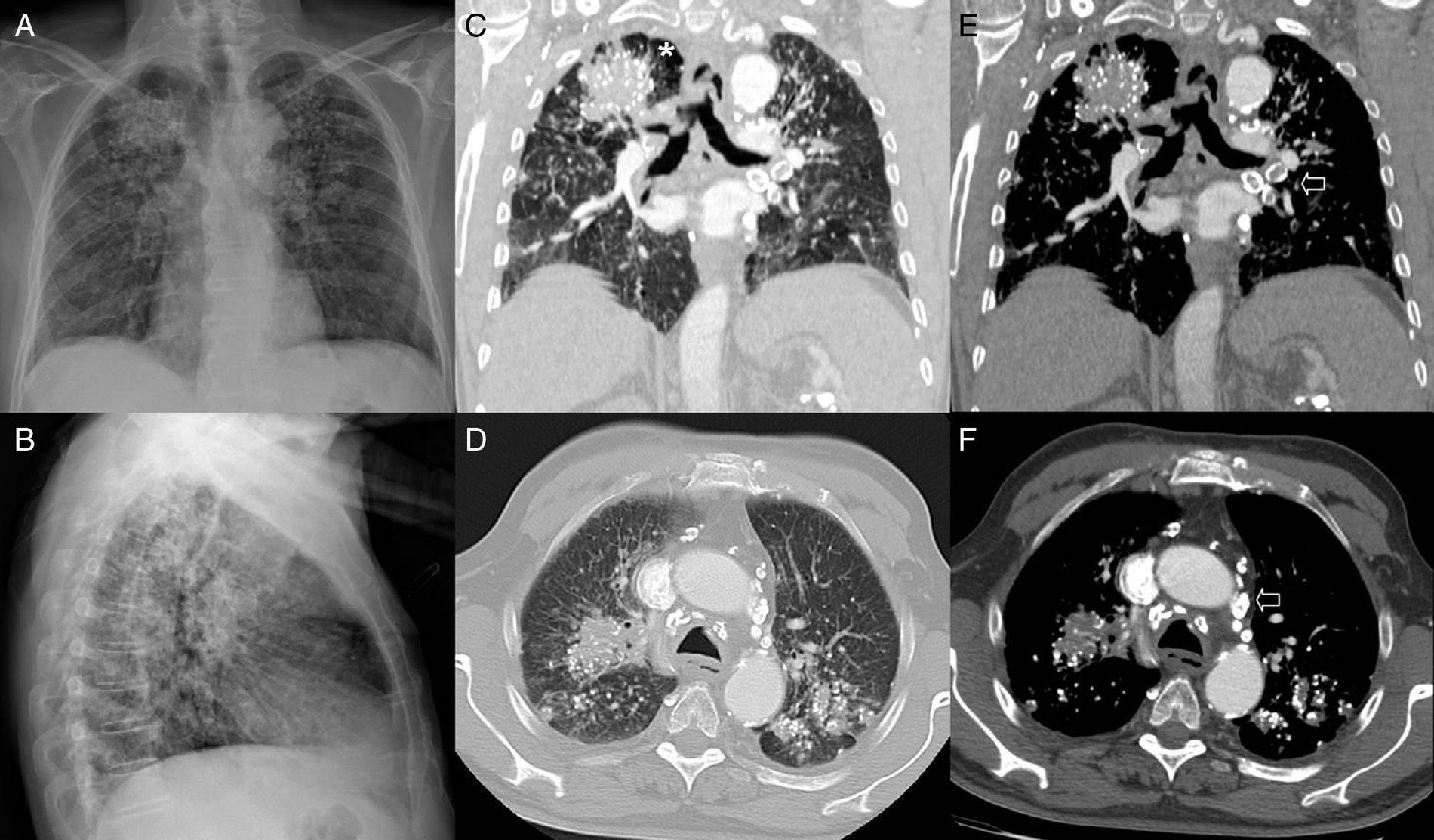
Chest X-ray revealed a diffuse bilateral nodular pattern with posterior opacities in the upper lobes associated with volume loss, hilar retraction and compensatory emphysema of the lower lobes, in addition to bilateral hilar adenopathies with peripheral “egg-shell” calcifications (Fig. 1A, B, E, and F).
Posteroanterior (A) and lateral (B) chest X-ray: bilateral posterior upper lobe opacities (visible in B), associated with volume loss, hilar retraction and compensatory emphysema of the lower lobes. Diffuse bilateral nodular pattern. Hilar adenopathies with peripheral “egg-shell” calcifications. Coronal (C, E) and axial (D, F) CT images in lung and mediastinal window, respectively: bilateral opacities in posterior upper lobe segments containing punctiform calcifications. Paracicatricial emphysema between right upper lobe opacity and adjacent pleura (asterisk). Multiple diffuse bilateral centrilobular nodules. Mediastinal and hilar adenopathies with “egg-shell” calcifications (arrows).
CT revealed opacities containing punctiform calcifications, along with paracicatricial emphysema between the right upper lobe opacity and the adjacent pleura (Fig. 1C and D).
These findings were consistent with progressive massive fibrosis. The patient was advised to quit smoking and symptomatic treatment with bronchodilators and N-acetylcysteine was started. The patient's respiratory situation is currently stable.
Recommended bibliographyFerreira AS, Moreira VB, Ricardo HM, Coutinho R, Gabetto JM, Marchiori E. Progressive massive fibrosis in silica-exposed workers. High-resolution computed tomography findings. J Bras Pneumol. 2006;32:523–8.
González Vázquez M, Trinidad López C, Castellón Plaza D, Calatayud Moscoso del Prado J, Tardáguila Montero F. Silicosis: computed tomography findings. Radiologia.2012 [Epub ahead of print].
Please cite this article as: Bueno Palomino A. Fibrosis masiva progresiva en un extrabajador de limpieza mediante chorro de arena. Arch Bronconeumol. 2014;50:456–457.