Small cell carcinoma is a neuroendocrine poorly differentiated tumor that accounts for a considerable amount of lung cancer cases. However, its location in the trachea is rare. It represents 5–8% of primary tracheal tumors in the majority of cohorts.1–5
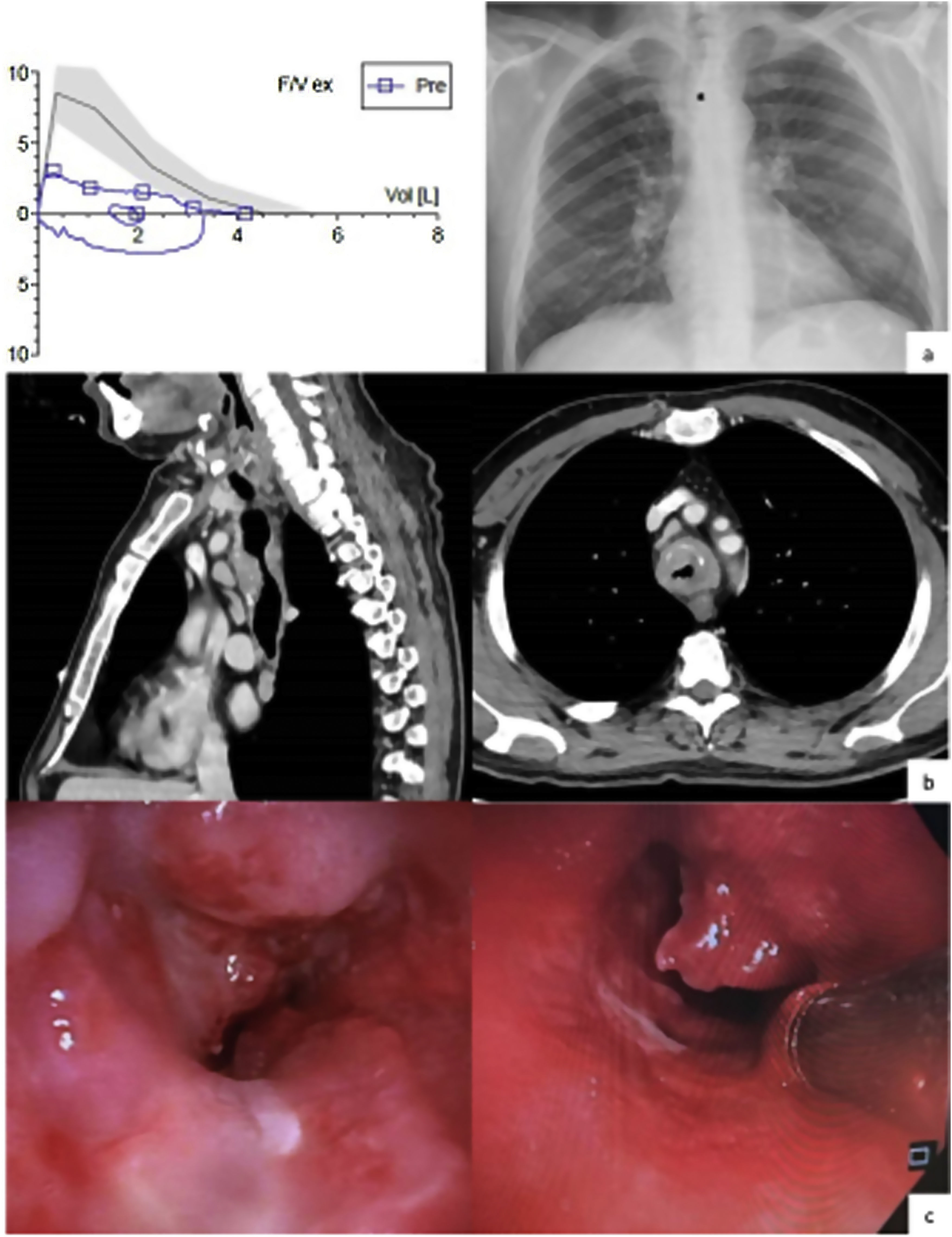
We present a 51-year-old man, an active smoker with a cumulative smoking rate of 50 pack-years and consumer of 80g of alcohol per day. His clinical record showed essential hypertension and hepatic steatosis. For several months he had experienced shortness of breath, oppressive chest pain, cough – sometimes accompanied by bloody sputum –, hoarseness, dysphonia and, later on, inspiratory stridor. The blood test and the arterial gasometry run in the emergency room showed polyglobulia and hypercapnic respiratory insufficiency. Initially, the patient was hospitalized in the respiratory ward and a spirometry and a chest X-ray were performed (Fig. 1a). The former proved a severe obstruction of the airway and a flattened expiratory phase in the flow-volume loop. As his condition worsened, he was admitted in the intermediate respiratory care unit and received non-invasive mechanical ventilation. A computerized thoracic tomography revealed a tracheal lesion that infiltrated its wall from its first ring to the carina, compromised 85% of its lumen and was in close relation with the aorta and the esophagus, as well as multiple adenopathies (Fig. 1b). A bronchoscopy was performed and a tumor with focal necrosis was removed (Fig. 1c). The anatomophatology analysis identified it as a small cell carcinoma. The cancer was staged as T4N2M0 (stage IV) after an extended radiological study. A second bronchoscopy was carried out in order to place a prothesis to lessen the symptoms caused by the obstruction. The patient is currently undergoing radiotherapy combined with cisplatin-based chemotherapy.
Our patient had sought medical assistance in two occasions and was first diagnosed with pneumonia and secondly with chronic obstructive pulmonary disease. The low sensitivity of the chest X-ray and the genericity of symptoms are responsible for the delayed diagnosis of tracheal tumors.1,4 Moreover, the incidence of these tumors is exceptionally low: 0.1 cases 100,000 person-years. This may be because particles, such as nicotine, are prompt to deposit in bronchus ramification areas, where the airflow is turbulent.3 In the adult population, 90% of tracheal tumors are malignant and generally result from the invasion of tumors originated in neighboring structures such as the larynx or the esophagus. Two thirds of primary tracheal tumors are squamous followed by adenoid cystic carcinomas. A heterogeneous group of benign and malignant neoplasms constitute the remain third.1,2 Small cell carcinoma usually affects males aged between 60 and 67 years old with a history of smoking. This does not differ from the population mostly affected by squamous cell carcinoma.1–4 However, the prognosis of the former is poorer, with only a 7% five-year survival rate.2 Age and lymph node involvement are independent prognosis factors.2 Treatment for small cell tracheal carcinoma is similar to other histological types. Radical surgery and adjuvant radiotherapy or chemoradiotherapy are of choice for localized tumors. In advanced stages, the latter are usually applied in addition to endoscopy excision and sometimes placement of tracheal prothesis to alleviate symptoms.1,2,4 Chemotherapy is commonly used against small cell tracheal tumors and has proven to prolong survival.2
FundingNone declared.
Conflicts of InterestAuthors have no conflicts of interest.