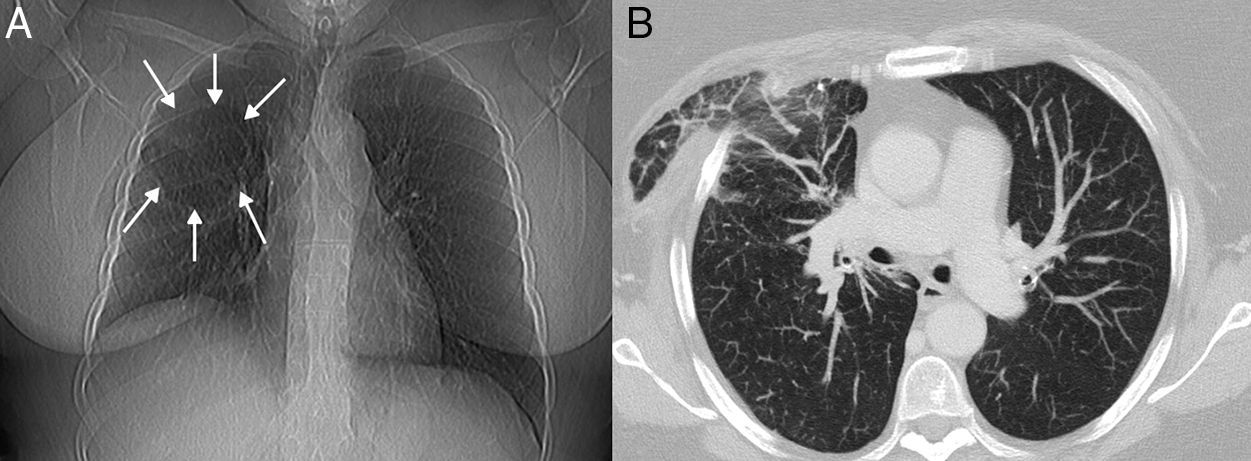
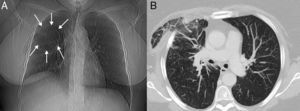
We report the case of a 63-year-old woman who had undergone surgery by thoracoscopy for lung cancer 4 years previously, consulting due to several episodes of hemoptysis and unspecific chest discomfort after a respiratory infection. Chest X-ray revealed a rounded radiolucent area in the right upper lung field (Fig. 1A). Chest computed tomography (CT) confirmed pulmonary parenchyma protruding through a defect in the anterior wall of the right hemithorax. The herniated pulmonary parenchyma showed increased ground glass density and interstitial thickening – findings consistent with venous congestion and edema (Fig. 1B). The patient underwent a surgical intervention to repair the chest wall defect with polypropylene mesh.
(A) Chest X-ray showing a rounded radiolucent area in the right upper lung field (arrows). (B) Chest computed axial tomography image (pulmonary parenchymal window) showing areas of ground glass attenuation and interstitial thickening in the herniated pulmonary parenchyma, consistent with areas of venous congestion and edema.
Pulmonary hernias can be congenital or acquired. Acquired hernias may be caused by traumatism or occur after surgery, spontaneously or due to chest wall or breast disease. Imaging procedures, particularly chest CT, can be used to confirm the presence of the pulmonary hernia, to precisely delimit both the hernial sac and the hernial orifice in the chest wall, and to rule out complications such as strangulation of the pulmonary parenchyma.1
Please cite this article as: Gorospe Sarasúa L, Ayala Carbonero AM, Fernández Méndez MA. Hernia pulmonar intercostal posquirúrgica. Arch Bronconeumol. 2016;52:332.