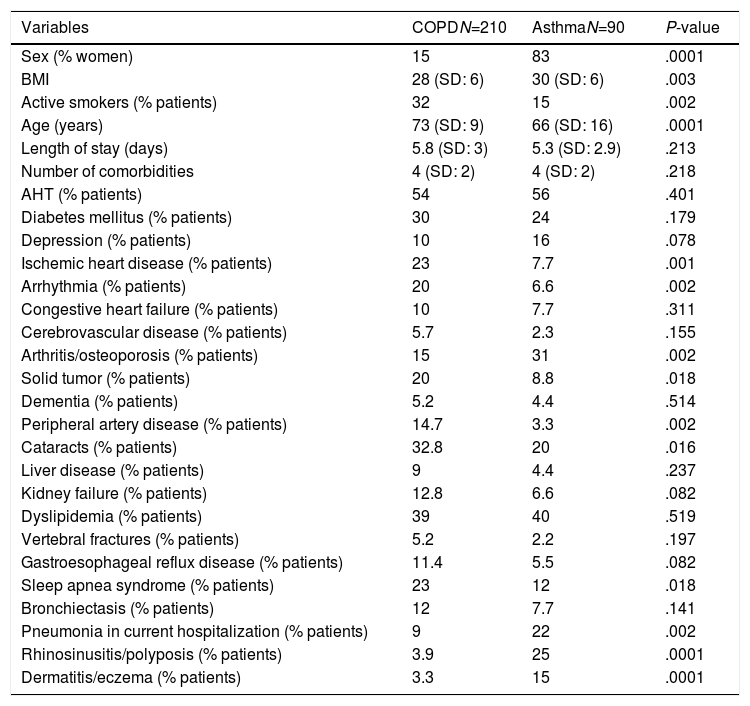
We recently conducted a systematic retrospective chart review of patients hospitalized with asthma or COPD during a 1-year period in the respiratory medicine department of our hospital (which attends a population of 276429 inhabitants), gathering information about their associated comorbidities. The sample consisted of 300 patients, 210 (70%) admitted with a diagnosis of COPD (30%) and 90 with a diagnosis of asthma. Women predominated among the asthma patients (83% vs 15%; P: .0001), their body mass index was higher (30±6 vs 28±6; P: .003), they were younger (66±16 years vs 73±9; P: .0001), and there were fewer smokers (15% vs 32%; P: .002). We found that comorbidities were very common in both groups (4±2 comorbidities/patient), the most prevalent in both groups being similar: hypertension, obesity, dyslipidemia, and diabetes (Table 1). It is of particular interest to see that the reason for admission among a significantly greater percentage of asthmatics was pneumonia: 22% vs 9% in the COPD group (P>.002). Unfortunately, we do not have patient data on the use of corticosteroids or on their immunization status.
Demographic Characteristics and Comorbidities of Asthma and COPD Patients.
| Variables | COPDN=210 | AsthmaN=90 | P-value |
|---|---|---|---|
| Sex (% women) | 15 | 83 | .0001 |
| BMI | 28 (SD: 6) | 30 (SD: 6) | .003 |
| Active smokers (% patients) | 32 | 15 | .002 |
| Age (years) | 73 (SD: 9) | 66 (SD: 16) | .0001 |
| Length of stay (days) | 5.8 (SD: 3) | 5.3 (SD: 2.9) | .213 |
| Number of comorbidities | 4 (SD: 2) | 4 (SD: 2) | .218 |
| AHT (% patients) | 54 | 56 | .401 |
| Diabetes mellitus (% patients) | 30 | 24 | .179 |
| Depression (% patients) | 10 | 16 | .078 |
| Ischemic heart disease (% patients) | 23 | 7.7 | .001 |
| Arrhythmia (% patients) | 20 | 6.6 | .002 |
| Congestive heart failure (% patients) | 10 | 7.7 | .311 |
| Cerebrovascular disease (% patients) | 5.7 | 2.3 | .155 |
| Arthritis/osteoporosis (% patients) | 15 | 31 | .002 |
| Solid tumor (% patients) | 20 | 8.8 | .018 |
| Dementia (% patients) | 5.2 | 4.4 | .514 |
| Peripheral artery disease (% patients) | 14.7 | 3.3 | .002 |
| Cataracts (% patients) | 32.8 | 20 | .016 |
| Liver disease (% patients) | 9 | 4.4 | .237 |
| Kidney failure (% patients) | 12.8 | 6.6 | .082 |
| Dyslipidemia (% patients) | 39 | 40 | .519 |
| Vertebral fractures (% patients) | 5.2 | 2.2 | .197 |
| Gastroesophageal reflux disease (% patients) | 11.4 | 5.5 | .082 |
| Sleep apnea syndrome (% patients) | 23 | 12 | .018 |
| Bronchiectasis (% patients) | 12 | 7.7 | .141 |
| Pneumonia in current hospitalization (% patients) | 9 | 22 | .002 |
| Rhinosinusitis/polyposis (% patients) | 3.9 | 25 | .0001 |
| Dermatitis/eczema (% patients) | 3.3 | 15 | .0001 |
AHT: arterial hypertension; BMI, body mass index; COPD: chronic obstructive pulmonary disease; SD: standard deviation.
The literature often emphasizes the adverse effects of both systemic and inhaled steroids. Evidence is available on the risk of pneumonia in patients with COPD who continue treatment with inhaled corticosteroids, but fewer publications address the issue in asthma patients.1 However, a recent study analyzing the adverse effects of systemic corticosteroids in a broad population of asthmatic adults in the United Kingdom2 found that the most frequent adverse effects are, in fact, infections. Asthmatics must often take both inhaled and oral corticosteroids, and perhaps we need to keep in mind, much more than we do in practice, that this population is at high risk of developing pneumonia.3 While pneumococcal vaccination is specifically recommended in patients with COPD (emphysema or chronic bronchitis),3 the Spanish asthma management guidelines (GEM) call for studies to definitively establish their indication in asthma patients.4 Some authors believe that these guidelines are outdated with respect to pneumococcal vaccination.5
This issue, in our opinion, should be taken into account when reviewing an asthma patient in the office, and we should consider taking preventive measures against pneumonia, especially in obese women with hypertension and dyslipidemia. These patients have an increased risk of not only pneumonia but also hospitalization for pneumonia, and pneumonia is currently a frequent cause of admission in asthmatics, more so even than in patients with COPD.
Please cite this article as: Cabanes L, Valentín V, Martinez Moragón E. Neumonía en asmáticos: ¿le estamos prestando suficiente atención?. Arch Bronconeumol. 2019;55:397–398.