Since time immemorial, humans have always desired to foretell the future. In ancient days, the prophets, intermediaries between humans and gods, became the ruling elite, since they were best placed to make the right decisions based on their revelations. This “prophetization” is what we now call prospective evaluation – a process that, though not prophetic, does have a common aim with the ancient prophetic traditions: to know where the future will lead us and to make better decisions in the here-and-now. Nowadays, we depend on the opinions of experts articulated via systematized mechanisms of reflection. For example, many countries, including Spain, have set up “foresight units” dedicated exclusively to forward planning: Canada (Policy Horizons), France (Centre d'Analyze Strategique), Finland (Foresight Unit), and the United Kingdom (Foresight Office), to name just a few. The future is not pre-determined, but neither is it a vacuum where we can move freely. Our very use of prospective methods clearly implies that the future we foresee is not neutral, but instead reflect particular desires, values, cultural assumptions, and worldviews.
At the end of 2019, the Committee on Quality and Innovation of the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) launched the Pneumology Project H2030, that aimed to “forecast” the future of respiratory health in Spain. We sought expert technical advice and began our collaboration with the Deusto Business School Health team at the Universidad de Deusto. This partnership has resulted in the report entitled: “Pneumology Project H2030: A prospective overview of respiratory health in Spain.”1 Our goal was not only to predict the future, but also to systematically analyze the available empirical evidence to identify potential challenges and opportunities in respiratory medicine.
The document was prepared primarily using the Delphi method, with the participation of 70 qualified experts nominated by both partners. The predictive capacity of Delphi is based on the systematization of the judgment of experts selected for their outstanding profiles and their key knowledge of the problem in question.2 This method is effective for consulting expert groups on future developments in their respective fields.3
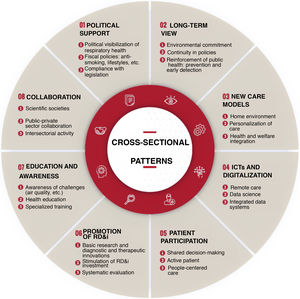
A series of factors was proposed (see Fig. 1), and we highlight the 9 that were awarded the highest impact scores (9–10) in 2030 by most experts (> 50%). These include, in order of importance: healthy lifestyle, public policies on smoking, the role of nursing, air quality, population aging, Covid-19 and other pandemics, ratio of specialist physicians, new models of remote care, and climate change.
A more detailed analysis revealed that 6 of the 9 factors with the greatest impact are elements that transcend the health system, and as such require measures and policies that go beyond the aegis of the health system alone. However, some factors do involve our own resources, such as the role of nursing staff, the ratio of specialist physicians, and the enhancement of remote care models, and these areas should serve as our waymarkers.
We have 10 years in which to exploit our strengths and correct our weaknesses.
Our strengths will improve as new technologies in respiratory health are developed and implemented. For example, by 2030,4 most people will have personal devices (smartphones, portable devices, air quality sensors, EEG monitors, molecular test kits, etc.) that will display signals, similar to the dashboard of a current car, with gauges and alarms, and automatically transmit data that will assist us in our mission to promote healthy habits and prevent as far as possible the onset and exacerbation of diseases. This capacity for self-diagnosis will develop along with the value of the tests endorsed by the scientific community and supported by patient associations who will act as decision-makers in health policies.
Our weaknesses, on the other hand – characterized by the uncertain economic picture and the small number of specialists – will require the implementation of a specific cross-sectional plan with nursing and physiotherapy departments to adjust staffing to the recommendations for the year 2030.
To tackle threats ranging from political instability and climate change to population aging, this report recommends promoting training in the management of multidisciplinary care teams involving primary care, internal medicine, geriatrics, and respiratory home hospitalization to improve the management of chronicity.
The data extracted suggest that the situation we are currently experiencing is an opportunity to highlight the importance of respiratory health and to include respiratory health in the general culture.
In short, favorable trends for respiratory health in 2030 have been detected, including advances in therapeutic innovations, the impact of prevention strategies and policies to promote healthy living habits, and new management models. Nevertheless, we will have to face major challenges resulting from population aging, air quality, and future pandemics.
Please cite this article as: Egea Santaolalla CJ, Jimenez-Ruiz CA. Proyecto neumología H2030: nuestro future. Arch Bronconeumol. 2021;57:447–448.