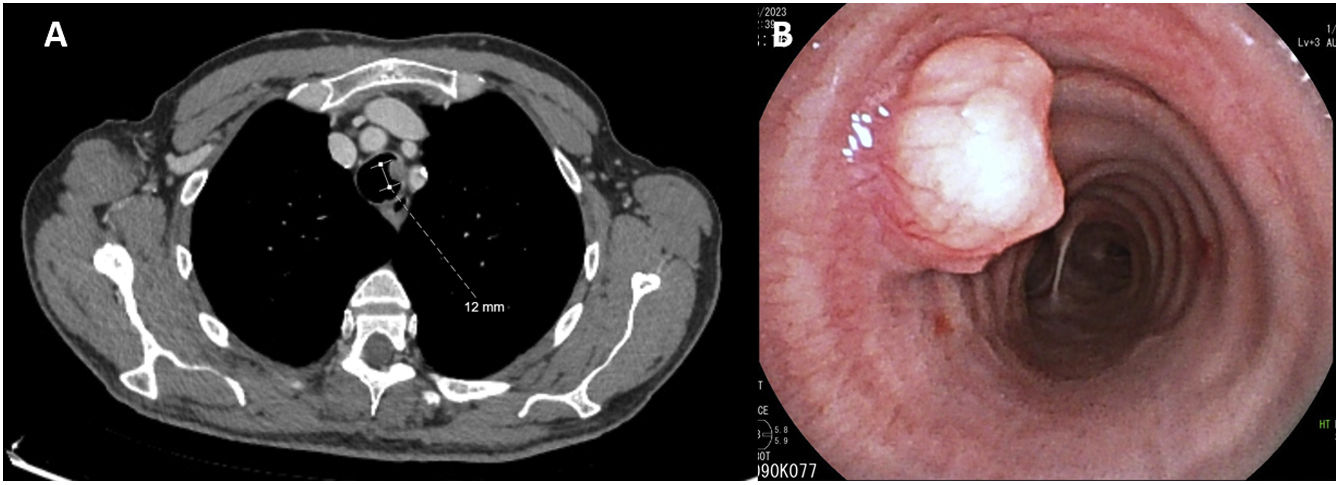
A 66 year-old male with a history of smoking (35 pack-year units) and gastric adenocarcinoma was referred to a Pulmonology consultation because of abnormal imaging findings. During routine follow-up, thoraco-abdominal computorized tomography was performed, revealing a polypoid lesion in the middle third of the trachea, with a maximum diameter of 12mm (Fig. 1A). He was asymptomatic and had a normal physical examination. Flexible bronchoscopy was performed, confirming the presence of an intra-luminal, highly vascularized polypoid lesion in the middle third of the trachea (Fig. 1B). Biopsies were performed, providing the diagnosis of a pleomorphic adenoma. After multidisciplinary discussion the patient was referred to Thoracic Surgery; segmental tracheal resection was successfully performed.
(A) Thoracic computorized tomography in axial plane demonstrating a polypoid lesion in the left side of the middle third of the trachea, with a maximum diameter of 12mm. (B) Endotracheal view of the trachea, confirming the presence of a vascularized polypoid lesion in the left wall of the middle third of the trachea.
Pleomorphic adenomas are the most common tumors of the salivary glands but are rare in the trachea (2–9%).1 Presentation is often delayed due to their insidious growth; radical treatment must be considered due to the high risk of recurrence.1,2 Although surgical segmental resection has been the preferred option, bronchoscopic intervention, with the aid of electrocautery or argon-plasma coagulation has been described.1,3 Given the rarity of this entity, its clinical course and optimal follow-up remain undetermined. Local recurrence has been documented after more than ten years.2
Conflict of InterestsThe authors state that they have no conflict of interests.