We present a 71-year-old woman with a long-standing history of severe eosinophilic asthma (por controlled with ACT scale of 15) and nasal polyposis, with suspected poor adherence to treatment at follow-up.
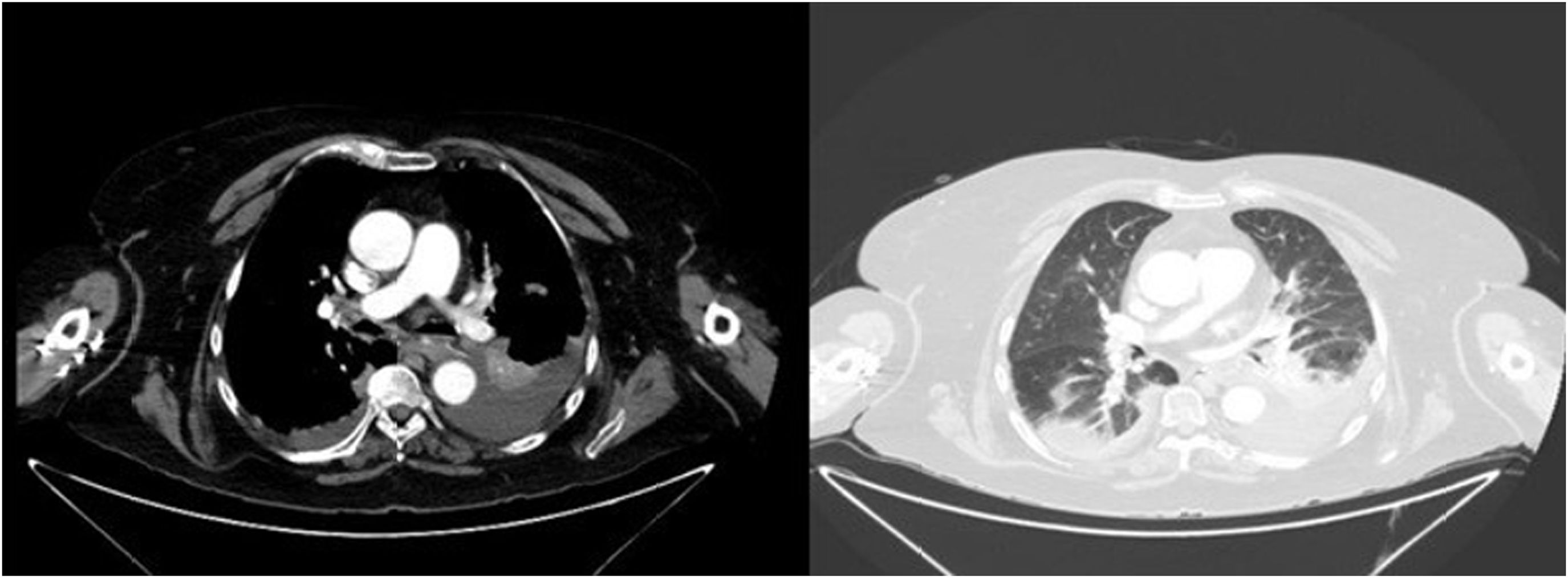
The patient was admitted to our hospital with clinical manifestations of cough and whitish expectoration. During physical examination, partial respiratory failure and semiology of asthmatic exacerbation with hypophonesis in lower pulmonary lobes were found. X-ray, and then chest CT, were requested showing consolidation in the upper lobes and bilateral pleural effusion (Fig. 1). Laboratory data showed no biochemistry alterations, NT-proBNP 262pg/ml, CRP 2.62mg/dl and leukocytosis 15,180/mcL (eosinophils 3.990/mcL, 27%). The ANAs, MPO-ANCA, PR3-ANCA, microbiology and serology were all negative (virus, bacteria and parasites).
In view of patient's poor respiratory progress, we performed a diagnostic thoracentesis, obtaining a yellowish non-hematic exudate with the following characteristics: pH 7.20, protein 6g/dl, glucose 214mg/dl, LDH 203U/L and leukocytes 6780/mcL (50% eosinophils). Cytology and microbiology were negative. It was decided to carry out a nasal turbinate biopsy, that showed eosinophilic infiltration of the corium. Polyneuropathy was ruled out.
EGPA was diagnosed classifying it as a nonsevere with a “Five Factor Score” (FFS) of zero. Treatment was started with prednisone 50mg and mepolizumab 100mg per day, progressively escalating to mepolizumab 300mg per day. After 6 months of full-dose treatment, the patient presented an excellent clinical and radiological improvement with complete resolution of eosinophilic pleural effussion (EPE).
According to the American College of Rheumatology (1990),1 more than 4 of the next 6 criteria are necessary for EGPA diagnosis: asthma, peripheral eosinophilia (>10%), neuropathy, sinusitis, extravascular eosinophilia and evanescent pulmonary infiltrates. Eosinophilic pleural effusion is a rare complication,2 with an incidence of 29% in patients with EGPA. Its characteristics have not been well described, having been defined by more than 10% eosinophil count, low pH and low glucose. Differential diagnoses of EPE include rheumatoid arthritis, bacterial pneumonia, tuberculosis, parasitosis, pharmacological, neoplasms, hematological disorders and, less frequently, certain vasculitis.
There is no standard therapy for the management of EGPA.3 Currently, the cornerstone of treatment consist of systemic glucocorticosteroids, with a relapse rate of 35%. In this context, immunosuppressive agents are used for maintaining remission. In spite of that, high dose of glucocorticoids and immunosuppressants may have long-term adverse effects. Recently, clinical benefits of mepolizumab have been demonstrated in patients with EGPA. MIRRA trial4 included patients with refractory EGPA treated with prednisone, demonstrating remission in 87% of patients treated with mepolizumab versus 53% in the placebo group. An European Observacional Study compared mepolizumab 300mg versus 100mg dose, showing both doses are associated with effective control of systemic EGPA manifestations.5
Therefore, mepolizumab is now a good therapeutic option for EGPA. It should be considered as a steroid-sparing drug used for maintenance of remission and control of non-organ-threatening flares, but not as a treatment for active organ-threatening disease.
Conflict of interestsThe authors state that they have no conflict of interests.