Thoracic duct cysts are lymph-filled dilatations that can be found in any portion of the thoracic duct, namely in supra or infra-diaphragmatic location.1 Supradiaphragmatic are typically found in the neck, whereas those in the mediastinal thoracic duct are quite uncommon.2 Its etiology is related to congenital or degenerative weakness of the duct wall.3 The cysts can be asymptomatic or, due to the pressure they can place on adjacent structures, be capable of causing symptoms such as cough, dyspnea, dysphagia, or chest discomfort. Usually, the clinical approach is conservative however, when reaches large dimensions, the treatment is surgical resection, to eliminate symptoms and prevent complications, such as spontaneous or traumatic rupture and chylothorax.3,4
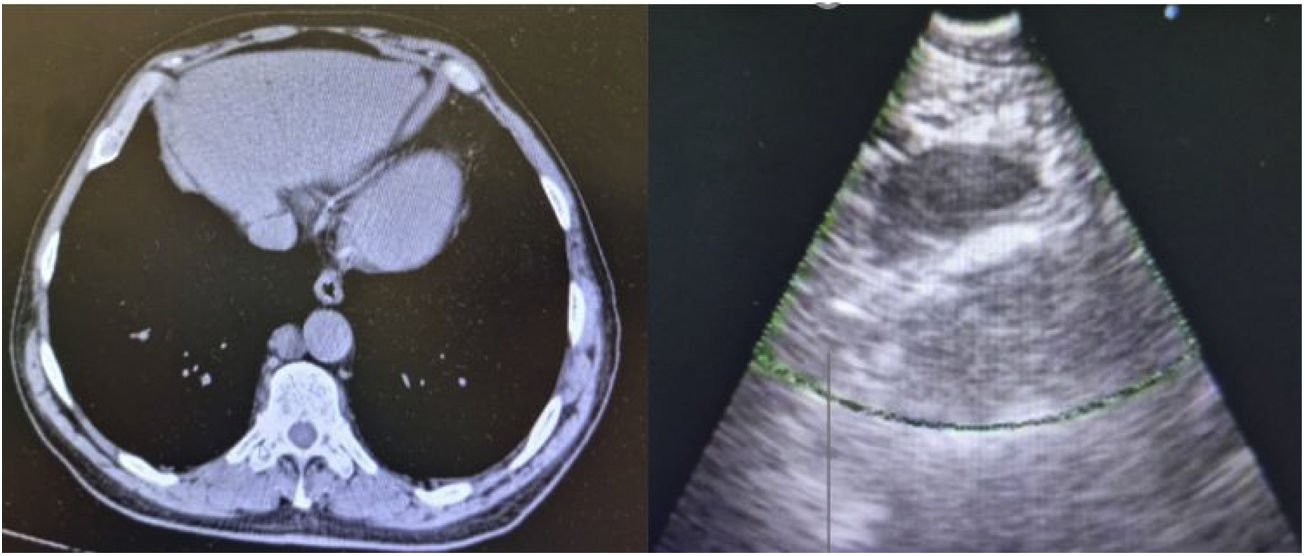
A 74-year-old male, non-smoker, was referred to a pulmonology appointment due to abnormalities in thoracic CT. He denied respiratory or constitutional symptoms and had history of prostate cancer, having been submitted to a radical prostatectomy with pelvic lymphadenectomy in 2014, type 2 diabetes mellitus, hypertension, and dyslipidemia. Medicated with atorvastatin, metformin, ramipril, acetylsalicylic acid and lercanidipine. In July 2021, control CT revealed stabilized lung micronodules and innocent lymph nodes; it was mentioned a 17mm short axis right para-aortic nodular formation, described as adenopathy. Patient performed blood laboratory analysis that revealed no alterations. Physical examination showed normal cardiopulmonary auscultation and no digital clubbing. Patient was referred to Portuguese Oncology Institute of Coimbra to perform an endoscopic ultrasound-guided fine needle aspiration puncture (EUS-b-FNA). Through echoendoscopy it was identified and punctured the mentioned right para-aortic formation, that was ovoid, well-defined, homogeneous and hypoechogenic. The material collected was a yellowish liquid which revealed high triglycerides concentration in laboratory analysis (424mg/dl). Normal results were obtained by immunophenotyping. The exam was performed without complications (Fig. 1).
The clinical importance of identifying thoracic duct cysts lies in their radiological misinterpretation as a pathological lesion, which can lead to an inappropriate and aggressive clinical approach. In the described case, the minimally invasively procedure, through EUS-b-FNA, allowed the lesion to be punctured and diagnosed reliably and safely. The collection of a yellowish liquid material, which laboratory analysis indicated a marked elevation of triglycerides, as well as a radiological location compatible to a mediastinal thoracic duct cyst, leaded to conclude that the formation corresponded to a cystic structure with this etiology. Due to small cyst dimensions and lack of symptoms, in this case the approach was conservative. Patient maintains follow up in pulmonology appointment.