A lymphangioma is a benign congenital malformation characterized by well-differentiated lymphatic proliferation, usually presenting as multicystic or sponge-like accumulation.1
Approximately 1% of lymphangiomas occur in the mediastinum.2,3 Lymphangiomas in adults is uncommon, but they most commonly occur in men and in the superior/anterior mediastinum.2,3 Posterior mediastinum seems to be a less frequent location.3
We report the case of a 35-year-old man who presented in April 2021 with a 24-h history of nausea, vomiting, fever, and elevated inflammatory markers. He reported pleuritic pain with years of evolution. Chest posteroanterior radiograph was normal. Whole-body computed tomography (CT) showed a low-density prevertebral heterogeneous mass involving the descending thoracic aorta and extending to the retroperitoneal fat and left perirenal space (Fig. 1a–c). A diagnosis of aortitis was suggested, and the patient was admitted. The echocardiogram was normal.
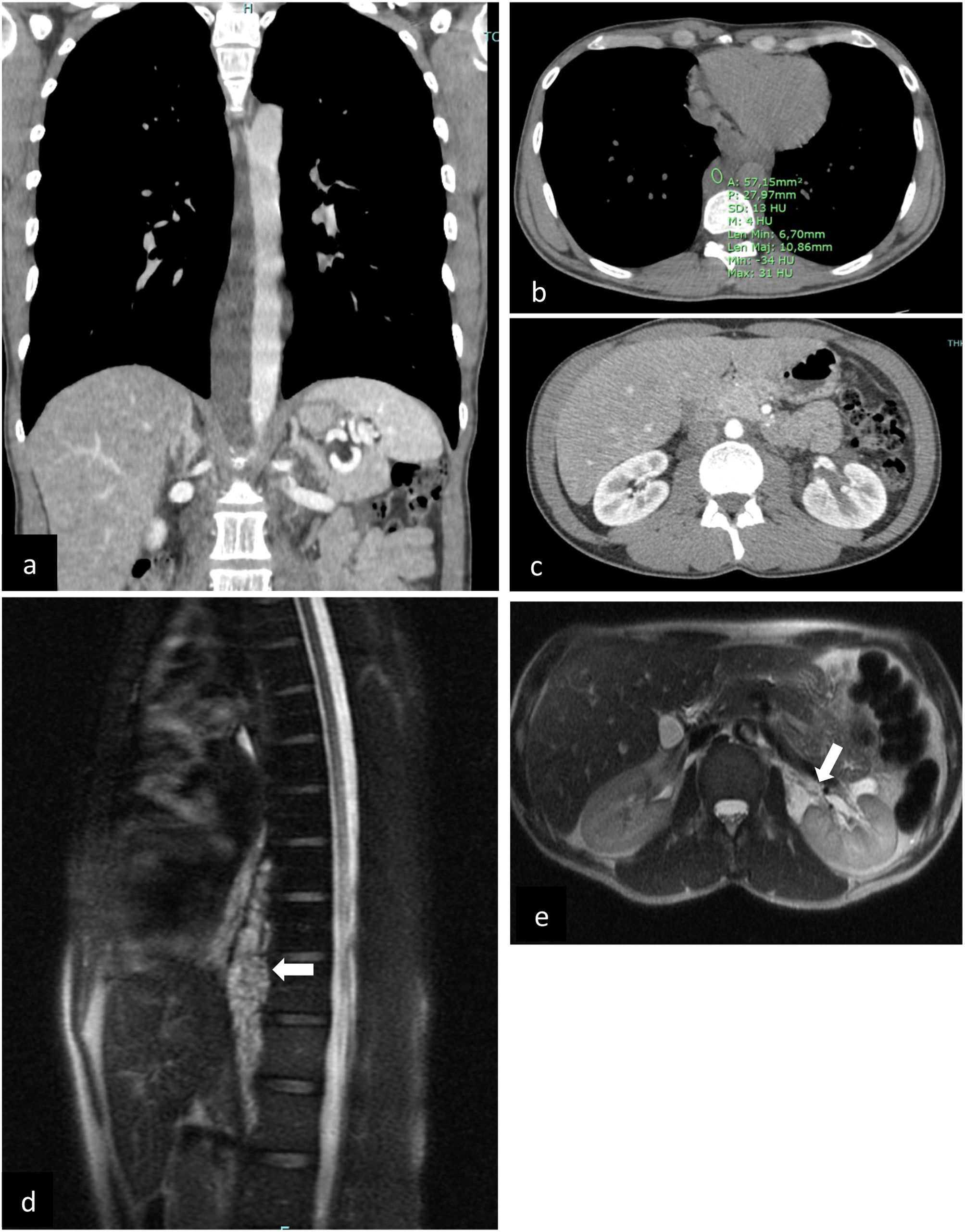
(a–c) (original images) – Whole-body CT – (a) coronal, contrast-enhanced (b) axial, unenhanced: prevertebral heterogeneous low-density (4 HU – fluid content) mass involving the thoracic aorta, from D6 to L1 (through diaphragm); (c) axial, contrast-enhanced: discrete heterogeneous density of retroperitoneal fat and central low attenuation areas in the left kidney; (d–e) (original mages) Chest-abdomen MRI – (d) MRI (sagittal): multiseptated serpiginous lesion in the posterior mediastinum/prevertebral (white arrow), forming a structure that molds to vascular structures (10.5cm in the craniocaudal diameter). (e) MRI (axial): left perirenal lesion molding to the renal hilum (white arrow), hyperintense on T2-weighted sequences, with multiloculated areas (equally hyperintense on T2).
Analysis of autoimmunity, antibody serology tests and immunodeficiency tests revealed no changes. Microbiological tests, including blood cultures, urine cultures, PCR test for SARS-CoV-2 and pneumococcal urine antigen test were negative.
Reviewing the CT images, it was possible to exclude the involvement of the aorta, since it was a mass of the posterior mediastinum that molded around the vascular structures without involving them. Lymphoproliferative disease, germ cell tumor and neurogenic tumor were considered the main possibilities.
Magnetic resonance imaging (MRI) was performed, showing a multiseptated serpiginous lesion in the posterior mediastinum/prevertebral, with a high signal on T2-weighted images, that molds to vascular structures. Additionally, there was a left perirenal lesion, T2-hyperintense, multiloculated, non-contrast-enhanced and unrestricted on diffusion sequences (Fig. 1d, e); adenopathy was not evident.
Upon reviewing the multiple exams, the most likely diagnostic hypothesis was incidental posterior mediastinal lymphangioma with extension to the perirenal region. A biopsy of the lesion was performed via endoscopic ultrasound. Flow cytometry of fine-needle aspiration was not compatible with lymphoma. The histology showed a benign vascular lesion with characteristics of lymphangioma, no signs of malignancy.
The acute symptoms were attributed to gastroenteritis.
A follow-up strategy was adopted, still with no complications.
The majority of lymphangiomas are diagnosed until 2 years of life,4 mostly as a mass in the neck or axilla.3 Thoracic lymphangiomas in adults are frequently asymptomatic, due to their slow growth and soft consistency, making diagnosis difficult. However, they can become symptomatic due to the compression of mediastinal structures.1,3 Infection, airway compromise, chylothorax and chylopericardium are described complications.4
Lymphangiomas are usually incidentally detected on radiology studies. On CT, they are well-defined, hypodense and non-enhancing lesions. MRI images show them as well-defined and fluid-filled, with heterogeneous signal intensity on T1 and hyperintense and non-enhancing on T2-weighted Images.4
A few reports of lymphangiomas that extend through the diaphragm have been reported.5
Other lesions, mostly cystic, that must be considered in differential diagnosis include congenital anomalies, hematomas, mediastinal abscess, teratoma, nerve sheath and benign vascular tumors, lymphoproliferative disorder and necrotic tumors.4
This lymphangioma's posterior mediastinal location and extension through the diaphragm, as well as its presentation in adulthood, are rare findings. Lymphangioma should be considered in the presence of cystic-like lesions of the mediastinum. Histological confirmation becomes essential for a definitive diagnosis and the exclusion of other pathologies, namely malignancy.
Ethical considerationsInformed consent was obtained from the patient for the publication of this article.
Conflict of interestNone to declare.