A 45-year-old smoker was referred for evaluation of recent onset streaky hemoptysis and a large cystic lesion in the left lower lobe (LLL). Presence of air trapping in LLL was observed on computed tomography scan of thorax. Prior to completion of diagnostic evaluation, the patient was lost to follow-up. On return after a two-month gap, ‘disappearance’ of the cyst was observed along with complete collapse of LLL. A fibreoptic bronchoscopy revealed presence of a tumor completely occluding the LLL main bronchus and biopsy confirmed presence of squamous cell carcinoma of lung. The temporal clinico-radiological profile suggested a check-valve mechanism resulting from endobronchial obstruction as the primary mechanism for cyst formation. This case highlights the need to consider malignant endobronchial obstruction as the likely etiology among heavy smokers presenting with symptomatic solitary lung cysts.
Hombre de 45 años de edad, fumador, que fue derivado para la valoración de un esputo hemoptoico (estrías hemáticas) y una lesión quística extensa localizada en el lóbulo pulmonar inferior izquierdo (LII). En la tomografía computarizada (TC) torácica se observó la presencia de atrapamiento aéreo en LII. Antes de completar la evaluación diagnóstica, el paciente se perdió para el seguimiento. Al regresar después de un intervalo de 2 meses, se observó la «desaparición» del quiste junto con el colapso completo del LII. La broncoscopia de fibra óptica reveló la presencia de un tumor que ocluía por completo el bronquio principal del LII y la biopsia confirmó la presencia de un carcinoma pulmonar de células escamosas. El perfil clínico-radiológico temporal sugirió un mecanismo de válvula como consecuencia de la obstrucción endobronquial como causa primaria de la formación del quiste. Entre grandes fumadores que se presentan con quistes pulmonares solitarios, sintomáticos, el caso descrito destaca la necesidad de considerar la obstrucción endobronquial maligna como la etiología probable.
Cystic lung lesions are radiological anomalies that are frequently observed. The majority are related with benign diseases. Malignant transformations of benign cysts are rarely observed.1–3 The formation of lung cysts is an exceptional presentation of primary lung cancer, and only a few clinical cases have been published.4,5 In this present article, we report the case of a patient who initially presented with a cyst in the left lower lung lobe detected on chest radiography. After the “disappearance” of the cyst and the complete collapse of the affected lung, the diagnosis of squamous cell lung cancer was established.
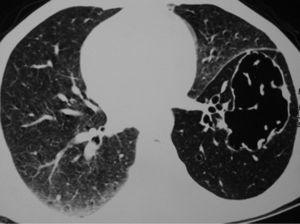
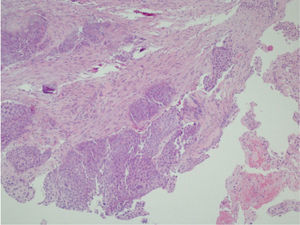
Clinical NotesA 45-year-old man requested an evaluation from his general practitioner after events of hemoptoic sputum and dry cough that had evolved over the period of one month. Consequently, he was sent to our hospital after a posteroanterior chest radiograph (Fig. 1) showed the presence of a cyst in the lower left lobe (LLL). In the initial evaluation, the patient reported a history of smoking of 26 pack-years. He also stated that a previous chest radiography study, done two years before at a systematic annual medical check-up, showed no anomalies. The patient had had no history of previous respiratory disease. Physical exploration revealed a reduction in the intensity of the vesicular murmur in the inter- and infra-scapular areas. Chest computed tomography (CT) showed an irregularly shaped, thin-walled cyst as well as a general reduction in LLL attenuation (Fig. 2). A bronchoscopic study was programmed, but the patient was lost to follow-up. Two months later, the patient returned to our department due to worsened symptoms associated with anorexia and a weight loss of 4kg. Repeated thoracic CT (Fig. 3) demonstrated the complete collapse of the LLL, which contained a fluid-filled cyst that was also collapsed (black arrow). A mass was also observed in the left hilar region with the loss of the fat plane of the descending aorta. On bronchoscopy (Appendix A) we observed a proliferation in the left main bronchus that was 4cm from the carina and completely occluded the main bronchus of the LLL. Endobronchial biopsy demonstrated the presence of squamous cell carcinoma (Fig. 4). Later, the patient received 4 cycles of chemotherapy with docetaxel and cisplatin, followed by thoracic radiotherapy (sequential), as a combined treatment for non-small-cell lung cancer in stage IIIB. The disease continued to progress, and the patient died some 10 months after the diagnosis.
Lung cysts are radiological anomalies that are frequently detected by general practitioners, pulmonologists and radiologists. Unusual causes of lung cysts include infections, such as pulmonary tuberculosis (both active as well as cured),6,7 non-infectious lung diseases, such as pulmonary leiomyomatosis,8 as well as bronchogenic tumors.9,10 Bronchogenic carcinoma or the typical histologic types of lung cancer are rarely associated with the presence of cysts.11 We have previously described a case in which lung cancer presented with a clinical–radiological suggestive of pulmonary echinococcosis, a benign parasitic disease.12 In general, centrally located lung cancer has a tendency to present with segmental, lobar or complete pulmonary collapse, but rarely has it been described as a cause of cyst formation.4,5
Several different mechanisms have been proposed as being related with the incidence of thin-walled cysts associated with lung carcinoma, including the presence of a check-valve mechanism as a consequence of stenosis of the proximal bronchus by a tumor (growth), the extension of tumor cells throughout the alveolar walls, the excretion of the liquid content of the tumor center with ischemic necrosis, and a tumor that originates from the wall of a pre-existing lung cyst.5,13
It is important to mention that the obstruction of the affected main bronchus is only associated with a check-valve mechanism when it is incomplete, for instance giving rise to air trapping and consequently the formation of a lung cyst. A check-valve mechanism has also been described in the formation of cysts in other non-malignant lung diseases.6,7
In the index case, the presence of a normal thoracic radiograph 2 years before the current disease, the generalized reduction in the attenuation of the pulmonary parenchyma surrounding the cyst on initial thoracic CT and, later, the presence of a tumor that completely occluded the main bronchus of the LLL associated with its complete collapse, support the hypothesis of a check-valve component as the main mechanism of the formation of the cyst. Although the previous chest radiograph, obtained when the patient was asymptomatic 2 years before, was not available, it was documented as having been normal; therefore, even if it had been present at the time, it is unlikely that a cystic lesion like that observed on the current chest radiography would have gone unnoticed. Similarly, the time line of events in this patient (lost to follow-up over the course of 2 months) did not enable us to carry out bronchoscopy during the initial presentation when we began to evaluate the cyst in the LLL. It is probable that it would have demonstrated an incomplete obstruction of the main bronchus of the LLL and that it would have provided the basis for a direct visual confirmation of the endobronchial progression of the process over time, as it could have been compared with the later endobronchial obstruction. Nevertheless, it is also possible that, if a bronchoscopy had been performed and, consequently, an endobronchial biopsy had been taken during the initial presentation of the patient, a diagnosis would have been established earlier and, therefore, its progression towards total collapse of the LLL might have been prevented.
As far as we, the authors, are aware, the patient described is the first documented case in the literature published in English in which, as a consequence of a check-valve mechanism, a pulmonary cyst had “disappeared” as the bronchial obstruction progressed from incomplete to complete. Further along, the cyst was no longer visible radiologically when the lesion, together with its content, became part of the atelectasis of the LLL.
The didactic aspect of this case is that, in patients with import tobacco consumption histories and recent onset hemoptysis, chest radiography revealing a single cyst (a lesion that is generally considered benign in nature) may in fact reflect the presence of endobronchial obstruction due to lung cancer. Therefore, it is necessary for physicians to suspect that they may encounter a situation with such characteristics at some point in their career. If not diagnosed and treated during the initial presentation, it may ultimately progress to complete atelectasis of the affected lobe/lung, as observed in the index patient. In addition, this can lead to the diagnosis later being established when the disease is advanced and no longer resectable, as occurred in this patient, which can ultimately affect the prognosis.
Conflict of InterestsThe authors declare having no conflicts of interest.
Additional material for this article may be consulted in its electronic version at doi:10.1016/j.arbres.2011.06.019.
Please cite this article as: Singh N, Bal A. Quiste pulmonar causado por un carcinoma broncogénico de localización central. Arch Bronconeumol. 2012;48:99-101.