Various diseases may present as cavitary pulmonary nodules, ranging from benign to malign diseases. A cavity is defined in Fleischner glossary as “a gas-filled space, seen as a lucency or low-attenuation area, within pulmonary consolidation, a mass, or a nodule”.1 The thickness of the cavity wall and symptoms may help differentiate.2 We present a case of a patient with metastatic adenocarcinoma of the lung presented as a multiple cavitary disease.
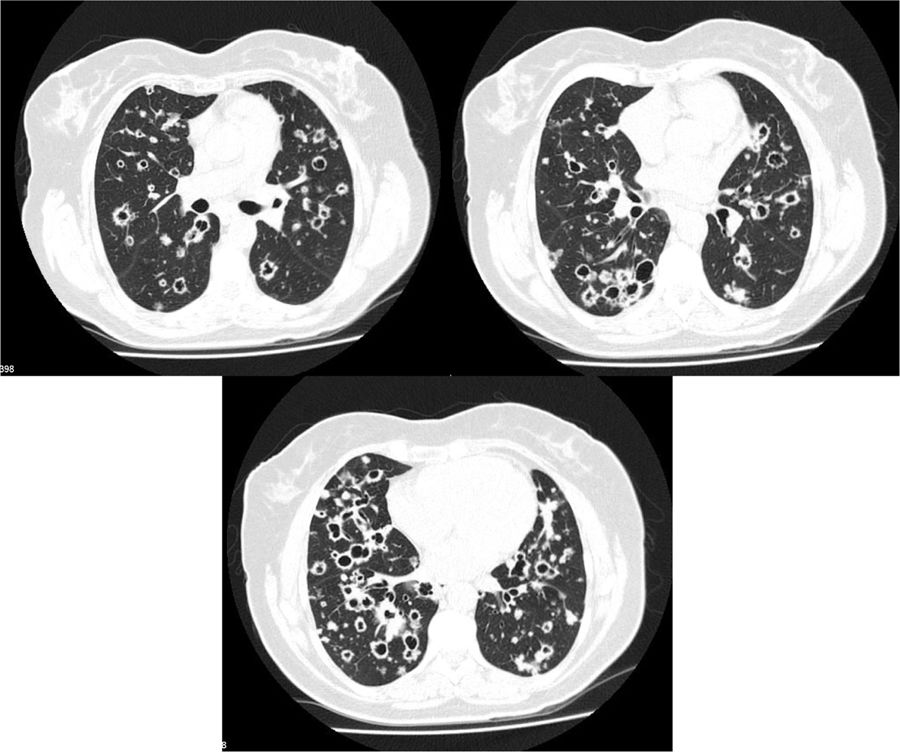
A 62 year-old female, former smoker (30 pack/year), with no relevant clinical history, presented with chronic dry cough, fatigue and weigh loss for 5 months. Her chest computed tomography (CT) scan showed multiple bilateral thin-walled air-filled cavities, with a diffuse distribution but basal predominance, round shaped but some of them with irregular borders, associated with centrilobular nodules (Fig. 1). She underwent flexible videobronchoscopy with no endoscopic abnormalities and a negative bronchoalveolar lavage (both cytological and microbiological analysis, including nucleic acid amplification test (NAAT) for Mycobacterium tuberculosis). Apart from positive antinuclear antibodies (ANA) and anti-Sjögren's-syndrome-related antigen A (SSA), blood analysis was irrelevant. The patient was then submitted to a surgical lung biopsy of the right lower lobe. Histological analysis of the biopsy showed multiple areas of mucinous adenocarcinoma. She was diagnosed with stage IV lung cancer and treated accordingly with chemotherapy.
Cavitation has been reported in up to 22% of primary lung cancer cases.3 It is believed that this phenomenon occurs due to rapid tumor growth that exceeds the blood supply with resultant central necrosis. Usually these cavitations have irregular or spiculated inner or outer margins, as well as thicker walls, but it has been found that some patients with lung cancer might also present with cysts or cavities with thin walls,4 which might lead to a misdiagnosis of a benign disease and delayed treatment.
The acute or chronic onset of symptoms might help narrowing the differential diagnosis; however, lung cancer might also present with acute symptoms of a concomitant a respiratory infection and lung abscess might be presented with chronic symptoms of weight loss and anorexia. There are, however, some radiologic findings that can help: rim enhancement of the walls on contrast-enhanced CT scan suggests abscess and satellite nodules might occur in infectious etiologies.5
Traditionally, squamous cell carcinoma was the most frequent histology found in cavitated tumors; however, an increasing number of adenocarcinomas have been found to form cavitations.6 Despite cavitation of primary lung cancer being relatively common, cavitation of lung metastases is infrequent. Only 4% of lung metastases cavitate,7 which makes this case a rare presentation of stage IV lung adenocarcinoma.
The differential diagnosis of a cavitary lung disease is challenging. Radiologic findings may help distinguish benign from malign disease, but a high suspicion of neoplasm is essential for preventing misdiagnosis.