We report the case of a 50-year-old woman, former smoker with no significant history who attended the emergency room with a 2-month history of a sensation of abdominal distension and hyporexia. She reported dry cough and hypogastric discomfort, with a weight loss of 2kg during this period, with no other clinic symptoms. Physical examination revealed ascites and the chest X-ray showed right pleural effusion.
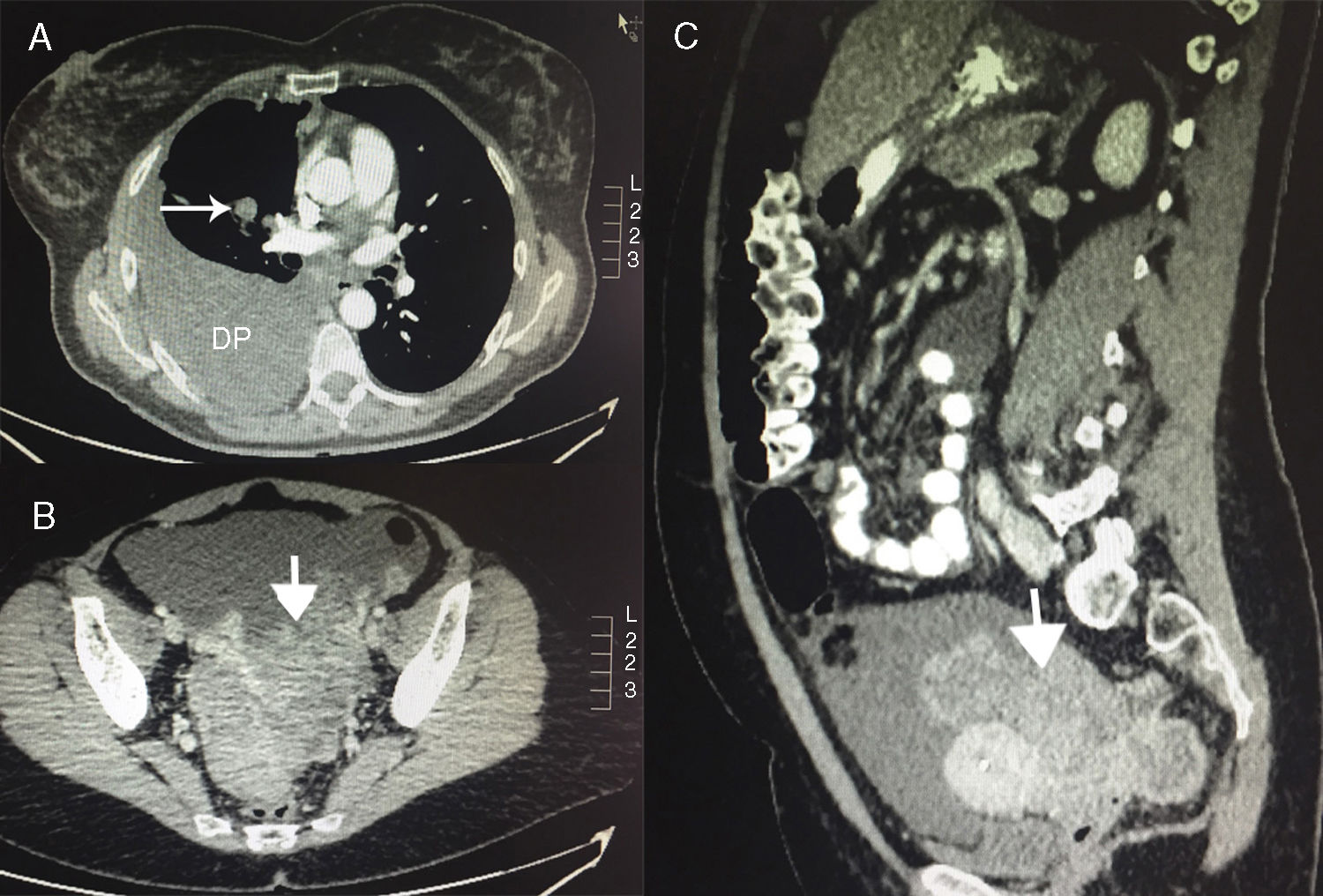
Chest-abdominal-pelvic computed tomography (Fig. 1) showed a solid, heterogeneous mass measuring 13.7×8×5.4cm in the pelvic cavity, avoiding the uterus and rectum, consistent with a neoplastic ovarian tumor, along with pleural effusion, 3 pulmonary nodules, and other nodules in the right paracardiac fat, ascites and nodular masses consistent with peritoneal carcinomatosis, metastatic involvement in 3 right costal arches, and other liver lesions consistent with metastasis. The presumed radiological diagnosis was ovarian cancer with abdominal and thoracic dissemination.
Pathology studies were performed: pleural effusion cytology found suspected malignant cells, and ascitic fluid cytology was consistent with metastatic adenocarcinoma probably of pulmonary origin according to immunohistochemistry (positive for CK7, EMA, TTF-1, napsin-A and CEA; low irregular p53 intensity, negative for CK20, WT1, GATA3, CDX2, PAX8 and thyroglobulin). Cytology of both the bronchial aspirate and transbronchial biopsy obtained during bronchoscopy was negative. CT-guided biopsy of the pelvic mass confirmed the pulmonary origin of the tumor (positive for CK7, TTF-1 and napsin-A, intense focal positivity for CEA, and weak focal positivity for p53; negative for CK20, PAX8, Cdx-2, WT1 and RE). The final diagnosis was poorly differentiated mucosecretory signet-ring adenocarcinoma consistent with a primary lung tumor (with no KRAS mutation and no expression of EGFR mutations, but positive for ALK-1 staining by immunohistochemistry and FISH). The final diagnosis was Krukenberg tumor originating from a lung adenocarcinoma. Thoracentesis and paracentesis were performed for symptomatic relief during the diagnostic process. Currently, the patient is receiving treatment with crizotinib, which is well tolerated. Follow-up CT showed clear radiological improvement, with practically complete resolution of the metastatic pleural component and reduced effusion, disappearance of the right parahiliar mass, no new lesions in the lung parenchyma, and resolution of the masses in paracardiac fat. Hepatic metastases were no longer visible in the abdomen, with improvement of ascites and peritoneal carcinomatosis. However, persistent bone involvement and pelvic mass were observed, although considerably decreased in size.
Krukenberg tumor is malignant metastasis to the ovary of mucosecretory signet-ring adenocarcinoma that usually originates from a gastrointestinal tumor and more rarely from other sources. It represents 1%–2% of all ovarian tumors.1,2 Gastric and colorectal cancers collectively account for almost 90% of cases.1 Other less common primary sites are breast, appendix, small intestine and endometrium. Lung cancer rarely causes ovarian metastases (scarcely 2%–4% of cases).3,4 Lung tumors that metastasize to the ovary are most often small cell disease (up to 40%–45% of cases).3–5 The exact mechanism of metastatic spread to the ovaries is unknown.1,6 The most common histopathological finding is adenocarcinoma with signet-ring mucosecretory cells. Clinically, patients may be asymptomatic or have non-specific symptoms depending on tumor involvement.1,2,6 Ascites may be observed in up to 39% of cases,6 as was the case in our patient. Despite the fact that studies have been performed to determine the typical immunohistochemical profile of this type of involvement, no single expression has been defined due to widely varying patterns.7 Nevertheless, napsin-A is a useful marker for differentiating primary lung adenocarcinomas from adenocarcinomas originating in other organs, and, in conjunction with TTF-1, increases the sensitivity and specificity of tests identifying the origin of metastatic lung adenocarcinomas.4 No specific therapeutic strategy has yet been defined. If the primary tumor is detected, it should be treated according to histology and staging.6 Prognosis is poor due to the metastatic nature of the disease, and mean survival is 14 months.1
In conclusion, we report the case of a Krukenberg tumor originating from lung adenocarcinoma, a very rare presentation in lung cancers, but one that should be taken into account in the differential diagnosis of ovarian masses.
Please cite this article as: Sota Yoldi LA, Vigil Vigil L, Martín Domínguez C, Antunes Parente B. Tumor de Krukenberg secundario a un adenocarcinoma de pulmón. Arch Bronconeumol. 2019;55:380–381.