Las guías clínicas de asma recomiendan la adopción de conductas de evitación alergénica. Para poder adoptarlas, los pacientes deben conocer las alergias que tienen. Sin embargo, este grado de conocimiento no ha sido hasta ahora evaluado. Los objetivos principales del estudio fueron determinar, en pacientes con asma alérgica: a) el grado de conocimiento de sus propias sensibilizaciones alérgicas; b) el porcentaje que conocen todas sus alergias y que, además, siguen normas de evitación alergénica (NEA) frente a todas ellas, y c) el eventual impacto de dicho grado de conocimiento sobre el nivel de control del asma.
Pacientes y métodosEstudio descriptivo, prospectivo y multicéntrico, con inclusión de 147 pacientes reclutados en 9 consultas externas de neumología. Tras verificar el diagnóstico previo de asma alérgica, se cumplimentó un cuestionario registrando los niveles de control y gravedad del asma, los resultados de los estudios de alergia previos, y la descripción y el número de sensibilizaciones alérgicas conocidas por el paciente y de NEA seguidas.
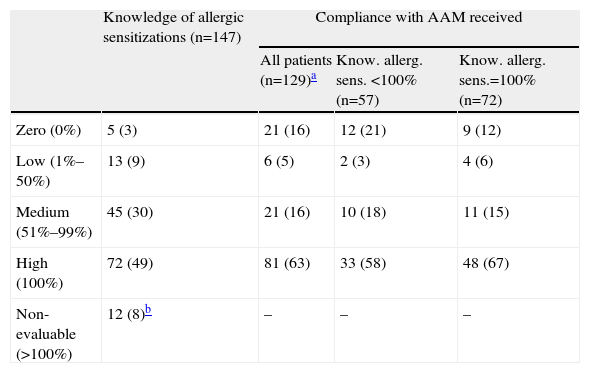
ResultadosTan solo 72 (49%) pacientes conocían todas sus sensibilizaciones alérgicas y únicamente 48 (33%) seguían, además, NEA frente a todos los alérgenos a los que eran alérgicos. No se demostró que existiera ninguna relación entre el grado de conocimiento de las propias sensibilizaciones alérgicas y el nivel de control del asma (p=0,544).
ConclusionesEl conocimiento global acerca de la naturaleza alérgica de su enfermedad, entre los pacientes asmáticos visitados en los servicios de neumología españoles, es insuficiente. Además, un adecuado conocimiento de las propias alergias no parece repercutir, por sí solo, en un mejor control del asma. Todo ello parece cuestionar la eficacia de las estrategias educativas actuales en este campo y, en consecuencia, estas deberían revisarse.
Asthma guidelines recommend the adoption of allergen avoidance measures (AAM). To do so, patients need to know their own allergies. However, this degree of knowledge has not yet been assessed. The aims of this study were to determine, in allergic asthma patients: (i) the degree of knowledge of their own allergic sensitizations; (ii) the percentage of those who knew all their allergies and, in addition, adopted AAM against all of them, and (iii) the possible impact of this degree of knowledge on the level of asthma control.
Patients and methodsDescriptive, prospective and multicentre study, including 147 patients from 9 Respiratory Medicine outpatient clinics. After confirming the previous allergic asthma diagnosis, a questionnaire was completed. It included asthma control and severity levels, results of previous allergy tests, and the description and number of allergic sensitizations known by the patients and AAM followed.
ResultsOnly 72 (49%) patients knew all their allergic sensitizations and only 48 (33%) were also following AAM against all the allergens to which they were allergic. No relationship was established between the degree of knowledge of their own allergies and the level of asthma control (P=.544).
ConclusionsOverall knowledge about the allergic nature of their disease among asthmatic patients attending Spanish Respiratory Medicine Departments is inadequate. Furthermore, a higher degree of knowledge of their allergies does not seem to lead, by itself, to better asthma control. Both findings seem to question the effectiveness of current educational strategies in this field and consequently, and they should be revised.
Exposure to allergens has been clearly shown to increase not only the risk of developing asthma,1 but also the morbidity of patients with allergic asthma.2 Likewise, it is well known that a combination of specific environmental control interventions is effective in significantly reducing the degree of exposure to allergens and consequently producing a clinical improvement in patients.3,4 Even though two systematic meta-analyses concluded that the efficacy of environmental control measures against house mites in patients with rhinitis5 is limited, and negligible in patients with asthma,6 the results of the latter study have been brought into question7 due to inappropriate selection of the studies included in the review. Finally, it has also been reported that good adherence to the recommendations for allergic avoidance reduces bronchial hyperactivity and morbidity in asthma.8,9
In 1997, the National Heart, Lung and Blood Institute developed their Guidelines for the Diagnosis and Management of Asthma,10 which state that “the first and most important step in controlling allergen-induced asthma is to reduce exposure to relevant indoor and outdoor allergens”. Similarly, in 2001 the American Academy of Asthma, Allergy and Immunology published a review article11 on the avoidance of allergens, in which they recommended that physicians inform their allergic asthma patients about strategies for avoiding exposure to domestic allergens. More recently, the latest review of the Spanish Guidelines for the Management of Asthma (GEMA)12 emphasizes that specific environmental control recommendations must be considered after confirmation of sensitization to the various allergens in each patient.
However, the hypothesis has emerged from routine clinical practice that patients who have already been diagnosed with allergic asthma, with or without associated rhinitis, often do not know for which allergens they tested positive in their allergy tests, or, at most, remember only partial information (e.g. “pollens” or “damp”). Consequently, a high percentage of patients with allergic asthma are likely to have inadequate disease control as a result of not adopting the allergen avoidance measures for allergens that they are sensitized to, but are unaware of.
The primary objectives of this study were to determine, in patients with allergic asthma: (a) their degree of knowledge about their allergic sensitizations, and very specifically, the percentage of patients who knew all of their sensitizations, (b) the percentage of patients who knew all their allergies, and who were also following all the allergen avoidance measures (AAM) as prescribed, and (c) the possible impact of the degree of knowledge of their allergic sensitizations on the level of asthma control. The secondary objective proposed for the study was the identification of other clinical or epidemiological variables that could possibly affect the level of asthma control (e.g. how closely the AAM were followed).
Patients and MethodsThis was a descriptive, prospective multicenter study which included 147 patients with allergic asthma (with or without associated rhinitis), aged between 18 and 80 years, seen in Respiratory Medicine outpatients in nine hospitals in seven different provinces in Spain (two hospitals participated in two provinces, Barcelona and Madrid), between February and October 2009. After calculation of the sample size required for this study (n=140, see below), the patient inclusion process concluded (due to organizational reasons of the study group) when it was established that this number had been reached. Between 11 and 21 patients were enrolled in the different participating sites, and between 13 and 23 in the various provinces, except in Barcelona, where a total of 40 patients were included.
Inclusion CriteriaPatients had to have a diagnosis of allergic asthma prior to inclusion in this study. The diagnosis was established after verifying that the patients met the clinical and functional disease criteria, previously described in the Global Initiative for Asthma (GINA).13 For the diagnosis of allergy, at least one positive result was required on the prick test14 or in the serum allergen-specific IgE antibody test (according to the positivity criteria of each laboratory). Patients had to sign an informed consent form before inclusion in the study.
Exclusion CriteriaThe following exclusion criteria were established: (a) prior diagnosis of bronchiectasis confirmed by computed tomography (CT) of the chest, (b) prior diagnosis of chronic obstructive pulmonary disease (COPD), even with bronchial hyperresponsiveness, or evidence of areas of emphysema on a previous CT, or (c) patients with evidence of cognitive deterioration or mental decline.
QuestionnairesAfter inclusion of each patient, the investigator completed a questionnaire, collecting clinical and epidemiological data, spirometry, prick test and serum allergen-specific IgE antibody test results, description and number of allergic sensitizations known to the patient, allergic avoidance guidelines recommended and followed, and levels of control [according to the Asthma Control Test (ACT)]15,16 and asthma severity [as established in the Spanish Guidelines for the Management of Asthma (GEMA)].12
Evaluation of the Degree of Patient's Knowledge About Their Allergic SensitizationsThe investigator asked the patients which specific allergies they knew they had from each of the following groups of allergens: dust mites, pollens, mold and animal dander. Patients were considered to be aware of a certain allergy if they confirmed that they were allergic to an allergen to which sensitization had been shown on the prick test or the serum allergen-specific IgE antibody test. Given the lack of previous studies using any type of classification scale for the allergic asthma patient's degree of knowledge about their own allergic sensitizations, we decided to define four arbitrary categories, depending on the percentage of allergies recognized by the patients, compared to those which had previously been demonstrated: (1) zero: 0%; (2) low: 1%–50%, (3) medium: 51%–99% and (4) high: 100%. This classification was selected on the basis of the hypothesis that if only two patient groups with a more polarized degree of awareness of their allergies were included (“high” and “zero”), the possible influence of this variable on the level of asthma control could be more easily demonstrated. In addition, as most patients had between one and four allergies (81%), the percentage of awareness of their allergic sensitizations would never be greater than 75% or lower than 25% for the vast majority of patients who would make up the subgroups defined as “medium” or “low”, respectively. As such, it was thought that in this way, a case could be made for the existence of a sufficiently clear differentiation of knowledge of their allergies between these two patient subgroups and those in the “high” and “zero” subgroups.
Evaluation of the Allergen Avoidance Measures Recommended to the PatientsThe investigator considered that patients had received AAMs against a certain allergen if, after questioning, they stated that they had received them in the past, for the four allergen groups described above: dust mites, pollens, mold and animal dander. Specifically, the patients were asked if they had received information from their doctor (or nurse) on the following particular aspects: measures for reducing exposure to dust mites (removing rugs, carpets, curtains, books or stuffed toys from the bedroom, use of anti-mite mattress and pillow covers, etc.), identification of the plants, grasses or trees producing the allergy-causing pollen, their pollination periods and barrier methods for reducing exposure (use of sunglasses or full helmet, closing car windows, etc.), measures for reducing exposure to pet dander (reducing or eliminating their presence in the home, use of antiallergenic lotions on the animals, etc.) and measures for reducing exposure to mold (avoiding damp in the walls of the home or damp environments).
Evaluation of the Degree of Follow-up of Allergen Avoidance Measures by the PatientsThe investigator asked the patients which AAM, among those recommended previously, they were currently following. Patients were considered to be following an AAM against a determined allergen if they reported that they had adopted at least one of the recognized effective methods for reducing exposure to that allergen (such as the examples described above), after being asked specifically about the measures for the four allergen groups: dust mites, pollens, mold and animals. As with the classification of the degree of knowledge about their allergic sensitizations, four classifications of compliance with the AAM received were defined, depending on the percentage of AAM that the patients stated that they were following, compared to the total number that they stated they had received in the past: (1) zero: 0%, (2) low: 1%–50%, (3) medium: 51%–99% and (4) high: 100%. Taking into account that the patients had received between one and four AAM (87% of those who received any AAM), the same argument used above for the classification of the degree of knowledge about their allergic sensitizations appears to be valid for this variable too.
Other Relevant Considerations(A) Different dust mites (D. pteronyssinus, D. farinae) and different molds (Alternaria, Aspergillus, Cladosporium, etc.) were considered a single allergy (as if it was one allergy to a group of allergens) when counting the number of allergies that the patient had or knew about, or the number of AAM that they had received or were currently following. Both animal dander and pollens were considered an independent allergic sensitization. (B) If a patient answered generically (e.g. “spring”) to any of the questions related with their allergies or AAM, they were first given the chance to answer more specifically, if they could, without the help of the investigator. If this was the case (e.g. the patient first answered “pollen” but then specified “grass pollen”), the more specific answer was recorded (in this case, “grass pollen” would be recorded). If the patient could not provide a more specific answer, their initial answers were recorded (e.g. “damp”, “pollen”, “dust”, etc.) in the questionnaire. In the latter case, when the known allergies or AAM followed were assessed, the responses “dust mites” and “dust” were considered valid if the patient was allergic to one or more dust mites and the response “damp” was considered valid if the patient was allergic to any mold (because taking measures to avoid exposure to “dust mites/dust” or “damp” confers lower exposure to the various dust mites or molds, respectively), but the generic response “pollen” was not accepted for allergy to one or more pollens (because knowledge of allergy to an unspecified pollen does not allow the patient to take allergen avoidance measures against one in particular in a certain pollination period).
Statistical AnalysisA descriptive analysis of the overall sample and the sample divided into the three asthma control groups (good, partial and poor control) was performed for all the variables collected. The values were expressed as frequencies and percentages. Mean values were compared between the three groups under consideration using one-way analysis of variance (ANOVA) for the quantitative variables and the Kruskal–Wallis test for comparative analysis of ordinal variables. The Pearson correlation was used for measuring the degree of association between qualitative variables. In all cases, the level of statistical significance was set at 5% (α=0.05). Data analysis was carried out using SPSS (version 18.0) software for Windows (SPSS, Inc., Chicago, IL, USA).
Calculation of Sample SizeA previous study found that 16% of hospitals in which asthmatic patients were treated had appropriate staff, equipment and educational programs.17 On this basis, we estimated that the percentage of positive responses for the primary variable (100% knowledge of their allergies) would not be higher than 10% in the best case scenario. So, taking into consideration that at least seven sites would be participating in the study, and assuming that each site would manage to include 20 or more patients, a minimum of 140 patients would be required. This would allow the calculation of a 95% confidence interval and the precision obtained (+/− epsilon) would be 5%. This level of precision was acceptable and in addition, since the estimates were low, it was very likely that more patients would eventually be included during the recruitment period, which would reduce the epsilon value, and consequently, increase precision.
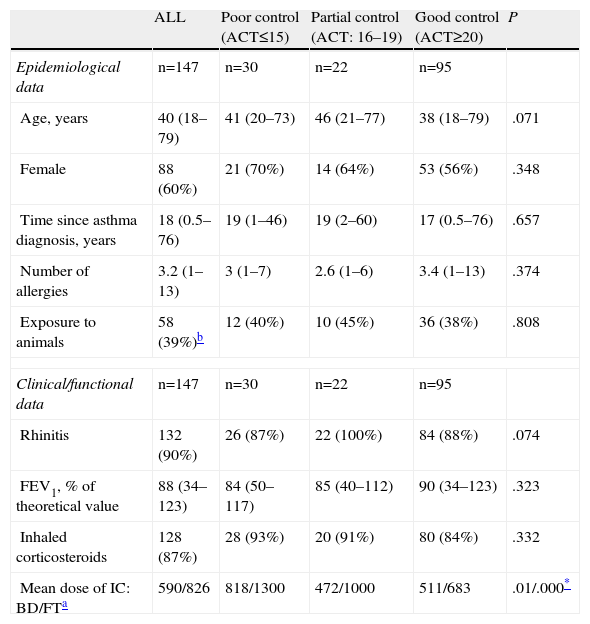
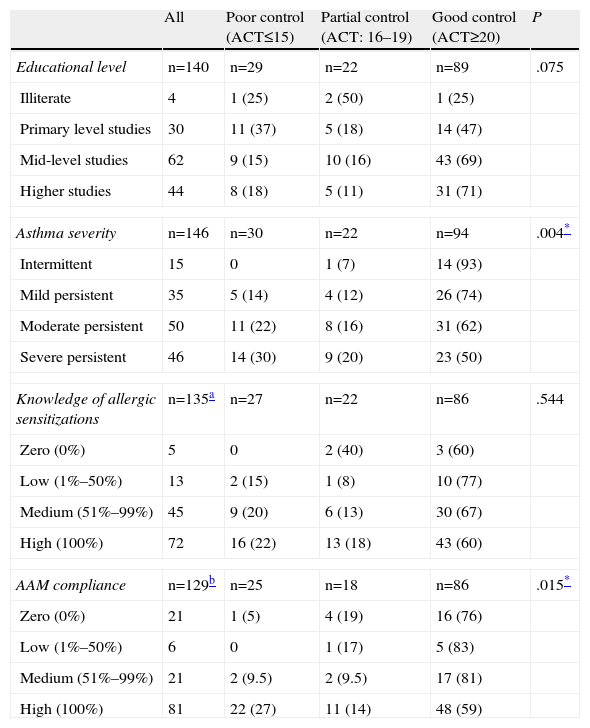
ResultsA total of 147 patients were included in the study, of whom 88 (66%) were women, with a mean age of 40 years (range: 18–79). The mean time since asthma diagnosis was 18 years (range: 0.5–76); this was classified as moderate persistent or severe persistent in 96 patients (65%). A total of 128 patients (87%) were receiving inhaled corticosteroids at the time of the study and the level of asthma control was good in 94 patients (65%). The last spirometry carried out in the patients before inclusion in the study showed an obstructive airways disorder (FEV1/FVC<70% and FEV1<80%) in 35 (24%). Clinical and epidemiological characteristics of the study population, and the three subgroups into which they were categorized (according to their level of asthma control), are described in more detail in Tables 1 and 2.
Epidemiological, Clinical and Functional Characteristics of the Study Patients by Level of Asthma Control.
| ALL | Poor control (ACT≤15) | Partial control (ACT: 16–19) | Good control (ACT≥20) | P | |
| Epidemiological data | n=147 | n=30 | n=22 | n=95 | |
| Age, years | 40 (18–79) | 41 (20–73) | 46 (21–77) | 38 (18–79) | .071 |
| Female | 88 (60%) | 21 (70%) | 14 (64%) | 53 (56%) | .348 |
| Time since asthma diagnosis, years | 18 (0.5–76) | 19 (1–46) | 19 (2–60) | 17 (0.5–76) | .657 |
| Number of allergies | 3.2 (1–13) | 3 (1–7) | 2.6 (1–6) | 3.4 (1–13) | .374 |
| Exposure to animals | 58 (39%)b | 12 (40%) | 10 (45%) | 36 (38%) | .808 |
| Clinical/functional data | n=147 | n=30 | n=22 | n=95 | |
| Rhinitis | 132 (90%) | 26 (87%) | 22 (100%) | 84 (88%) | .074 |
| FEV1, % of theoretical value | 88 (34–123) | 84 (50–117) | 85 (40–112) | 90 (34–123) | .323 |
| Inhaled corticosteroids | 128 (87%) | 28 (93%) | 20 (91%) | 80 (84%) | .332 |
| Mean dose of IC: BD/FTa | 590/826 | 818/1300 | 472/1000 | 511/683 | .01/.000* |
Presentation of results: quantitative values are expressed as mean value and, in parentheses, range; categorical variables are expressed as absolute number of patients meeting that criteria and, in parentheses, as a percentage of the total represented.
BUD=budesonide (n=61)/FT=fluticasone (n=65)/beclomethasone (n=2).
Education Levels and Asthma Severity, and Degrees of Patient Knowledge of Their Allergic Sensitizations and Compliance With Allergen Avoidance Measures (AAM) Received by Level of Asthma Control.
| All | Poor control (ACT≤15) | Partial control (ACT: 16–19) | Good control (ACT≥20) | P | |
| Educational level | n=140 | n=29 | n=22 | n=89 | .075 |
| Illiterate | 4 | 1 (25) | 2 (50) | 1 (25) | |
| Primary level studies | 30 | 11 (37) | 5 (18) | 14 (47) | |
| Mid-level studies | 62 | 9 (15) | 10 (16) | 43 (69) | |
| Higher studies | 44 | 8 (18) | 5 (11) | 31 (71) | |
| Asthma severity | n=146 | n=30 | n=22 | n=94 | .004* |
| Intermittent | 15 | 0 | 1 (7) | 14 (93) | |
| Mild persistent | 35 | 5 (14) | 4 (12) | 26 (74) | |
| Moderate persistent | 50 | 11 (22) | 8 (16) | 31 (62) | |
| Severe persistent | 46 | 14 (30) | 9 (20) | 23 (50) | |
| Knowledge of allergic sensitizations | n=135a | n=27 | n=22 | n=86 | .544 |
| Zero (0%) | 5 | 0 | 2 (40) | 3 (60) | |
| Low (1%–50%) | 13 | 2 (15) | 1 (8) | 10 (77) | |
| Medium (51%–99%) | 45 | 9 (20) | 6 (13) | 30 (67) | |
| High (100%) | 72 | 16 (22) | 13 (18) | 43 (60) | |
| AAM compliance | n=129b | n=25 | n=18 | n=86 | .015* |
| Zero (0%) | 21 | 1 (5) | 4 (19) | 16 (76) | |
| Low (1%–50%) | 6 | 0 | 1 (17) | 5 (83) | |
| Medium (51%–99%) | 21 | 2 (9.5) | 2 (9.5) | 17 (81) | |
| High (100%) | 81 | 22 (27) | 11 (14) | 48 (59) | |
Mean time since the last allergy tests performed (prick test and/or serum allergen-specific IgE antibody test) was 3.2 years (Me: 1.4, range: 0.3–46.6). A prick test for airborne allergens was carried out on all patients included in the study and was positive for one or more allergens in all except three cases; in these three patients, allergic sensitization had been confirmed with at least one positive result in the serum allergen-specific IgE antibody test (positive results for this test were also available for a further 33 patients).
The mean number of allergic sensitizations presented by the patients (see Table 1) was 3.2 (range: 1–13). Most patients showed one (20%), two (27%) three (20%) or four (14%) sensitizations. The most common allergic sensitizations were dust mites (D. pteronyssinus and/or D. farinae) in 95 cases (65%), grass pollens in 67 (46%), olive pollen in 62 (42%), cat in 48 (33%), dog in 37 (25%), plane tree pollen in 29 (20%) and mold en 29 (20%). However, the mean number of allergic sensitizations recognized by the patients was lower, 2.48 (range: 0–9).
The patients’ degree of knowledge of their allergic sensitizations is described in Table 3 (and also in Table 2, broken down into three patient subgroups classified by level of asthma control), but it should be noted that it was high in only 72 patients (49%). As can be seen in Table 2, no relationship was shown between the degree of patients’ knowledge of their allergic sensitizations and the level of asthma control (P=.544).
Study Population Distribution by Degree of Knowledge of Allergic Sensitizations and Compliance With Allergen Avoidance Measures Received.
| Knowledge of allergic sensitizations (n=147) | Compliance with AAM received | |||
| All patients (n=129)a | Know. allerg. sens. <100% (n=57) | Know. allerg. sens.=100% (n=72) | ||
| Zero (0%) | 5 (3) | 21 (16) | 12 (21) | 9 (12) |
| Low (1%–50%) | 13 (9) | 6 (5) | 2 (3) | 4 (6) |
| Medium (51%–99%) | 45 (30) | 21 (16) | 10 (18) | 11 (15) |
| High (100%) | 72 (49) | 81 (63) | 33 (58) | 48 (67) |
| Non-evaluable (>100%) | 12 (8)b | – | – | – |
Know. allerg. sens.: degree of patient knowledge of their allergic sensitizations.
With regard to the number of AAM received before inclusion in the study, 18 patients (12%) reported not having received any, 47 patients (32%) reported having received AAM for one allergen, 37 (25%) for two, 19 (13%) for three, 15 (10%) for four and 11 (7%) for five or more. The mean number of AAMs received was 2.06 (range: 0–12). A total of 74 patients (50%) stated that they had received the same number of AAM as allergic sensitizations that they showed.
The number of AAM that the patients said they were following was considerably fewer than the number of AAM received. A total of 40 patients (27%) reported that they were not following any AAM, 53 (36%) were following one, 26 (18%) were following two, 12 (8%) were following three, 9 (6%) were following four and 7 (5%) were following five or more. More specifically, the mean number of AAM followed by the 129 patients who stated that they had received one or more was 1.6 (range: 0–12) and 81 (63%) of these stated that they were following all of those received.
The degree of compliance with the AAM received by the patients, assessed according to the percentage followed, is described in Table 3 (and also in Table 2, broken down into three patient subgroups classified by level of asthma control), but it must be noted that this was zero or low in up to 21% of patients. In this case, the existence of an inverse correlation was shown, albeit weak, between the degree of compliance with the AAM and the level of asthma control (P=.015, Pearson correlation: −0.213). The same type of correlation with the level of asthma control could be identified for another two variables analyzed: the mean dose of inhaled corticosteroids and the level of asthma severity (see Tables 1 and 2, respectively). In other words, patients with poorer disease control had more severe asthma, required a higher mean dose of inhaled corticosteroids and appeared to follow the AAM more rigorously.
A sub-analysis of the degree of compliance with the AAM received by the 72 patients (49%) who knew all of their allergies (see Table 3) showed that 48 of them (67%), representing 33% of the complete study series, followed all those that they should, and 24 (33%) did not. In the second group of 24 patients who did not follow all the AAM that they should, eight (who represented 11% of those who knew all their allergies) could not do so because, among other reasons, they had not received all of them; the other 16 patients (who represent 22% of those who knew all their allergies) did not follow some or any of them, despite having received them all.
DiscussionThe principal finding of this study was that the overall knowledge of the allergic nature of their disease among patients with allergic asthma treated in Respiratory Medicine departments is clearly insufficient. More specifically, it shows that patients’ degree of knowledge about their allergies is suboptimal (only 49% of the patients studied knew all of their allergies) and that the behavior of only one-third of patients was perfectly appropriate to their disease, with a knowledge of all their allergies and compliance with AAM against all of the allergens to which they were sensitized. However, and in contrast with the concept proposed in our initial working hypothesis, it was not shown that the patients’ degree of knowledge of their allergic sensitizations alone affects their level of disease control.
As far as we are aware, there are no other studies previously published that have specifically assessed the degree of patients’ knowledge about their sensitization to airborne allergens in already diagnosed patients, nor the percentage of patients who are aware of and avoid the allergens to which they are sensitized. On the other hand, some studies do exist in which the degree of knowledge of the patients or their family members about other types of allergies or the adoption of certain types of avoidance behavior have been assessed. Gupta et al.18 found that the level of knowledge about food allergies was adequate among the parents of children with these allergies, but deficient in the general public, and in another study, by Joyce et al.,19 the frequency of adopting preventive methods by the mothers of children with a high risk of developing asthma or allergy was lower than desirable. Similarly, in a previous study, Wyatt20 analyzed the degree of knowledge about drug allergies in a population of 2500 patients attending emergency departments, and found that 15% of patients who declared some allergy did not know to which drug they were allergic; only 47% of the allergies reported by the patients that could be confirmed with their physicians were shown to be true, as they had been described. In short, the patients’ knowledge of their own drug allergies was deficient and imprecise.
The results of this study show that this suboptimal level of patient knowledge about their allergic sensitizations also occurs in a population of patients sensitized to airborne allergens who have been appropriately treated by pulmonologists (see Table 3). In our opinion, the fact that only 49% of these patients knew all their allergies is an unacceptably low percentage, particularly if we consider, in addition, the long mean time since diagnosis of their disease (17.6 years) and the short mean time since their last allergy study (3.2 years). It seems reasonable to think, moreover, that in environments outside the specialized clinics, where allergy studies are less accessible and common, and where time available for educating patients is much less or non-existent, the degree of patients’ knowledge of their allergies may be even worse than we have found here.
In any case, considering that the mean education level of this series was reasonably high (see Table 2), it seems unlikely that the patients’ deficient knowledge about their allergies can be totally attributed to the patients themselves. In this case, it is likely that part of the responsibility for this deficient knowledge can be attributed to the way in which the pulmonologists inform their patients and/or the time and infrastructures available for imparting this information.
One group that was difficult to evaluate was the 12 patients (8%) who said that they had more allergies than they actually had; one hypothesis for this may be that these are patients who are highly unaware of their real allergic situation, and follow deficient or erratic allergen avoidance measures, or else they are patients who are highly sensitive regarding their allergic disease and follow extraordinary, or even excessive, allergen avoidance measures. For this reason, we decided not to include these patients when analyzing the relationship between the degree of knowledge of their allergic sensitizations and the level of asthma control.
Of particular interest is the sub-analysis of the 72 patients (49%) who knew all their allergies. It is disappointing to see that, even in this patient subgroup, a considerable percentage (33%) also did not follow all the AAM they should (see Table 3), and in addition, 66% of these latter did not do so, despite having received AAM for all allergens to which they were sensitized (see Results). In a comparative group analysis, it was shown that the percentage of patients with perfect allergen avoidance practices was only slightly higher among patients who knew all their allergies (67%) compared to those who did not (58%) (Table 3). These data demonstrate that the simple fact of knowing all their allergies and the AAM that they should follow does not necessarily translate into compliance with these measures, as has been described in previous studies.21 The clearest evidence of this is that only 33% of all patients included in the study had the necessary knowledge and adopted the appropriate measures (following AAM) for their allergic disease.
In this respect, our results are consistent with those of Callahan et al.,22 who evaluated knowledge and practice of AAM for dust mite control in families with dust mite allergic asthma. In this study, the percentage of families who had received AAM, the percentage who showed knowledge of them and the percentage of the latter who actually applied any of those AAM was evaluated. This was all done by comparing two subgroups of these families, according to whether the patients had been seen by an allergologist or a pediatrician. The percentages obtained for each of the variables under study were 81%, 70%, and 60% for the first group and 49%, 18%, and 63% for the second. In short, the conclusion was that in spite of identifying a significantly greater knowledge of AAM among the families who had seen an allergologist, adherence to these measures and application of at least one of them in the home was similar in both groups (68% and 56%, respectively).
This study is the first to evaluate the impact of patients’ knowledge about their allergic sensitizations on the level of asthma control. Lack of knowledge about their allergies may lead to deficient avoidance measures regarding those allergens and, consequently, lead to poorer asthma control. However, our results seem to rule out this hypothesis (see Table 2). In our opinion, these results can most reasonably be explained by the existence of many other variables which determine whether or not patients follow certain AAM from the time that they know they are allergic to a certain allergen. These include, for example, the AAM that they actually receive (in this study, the mean number of allergic sensitizations presented by the patients was 3.2 but the mean number of AAM received was 2.06, 12% of patients stated that they did not receive any AAM for any allergen and only 50% of patients reported having received as many AAM as they had allergies) or the degree of patient compliance with these (adherence) (in this study, up to 21% of the patients who received any AAM followed only 50% of them or fewer). Moreover, in this study specifically, the fact that 87% of patients were on inhaled corticosteroid treatment at the time of their inclusion in the study, at high mean doses (see Table 1), may have affected the chances of finding significant differences in the level of asthma control according to the patients’ knowledge of their allergic sensitizations, since many patients may have achieved good disease control (65% of patients showed good control), regardless of their better or poorer compliance with AAM. In any case, independently of the causes that can be proposed for justifying the results obtained, these do seem to be consistent with the results of other authors,5,6 in that the adoption of isolated AAMs, not accompanied by more comprehensive educational programs, does not lead to better asthma control.
It is also worth mentioning the identification of three variables that showed some correlation with the level of asthma control. It is not surprising to see that a higher mean dose of inhaled corticosteroids and a higher level of asthma severity are related with poorer asthma control (see Tables 1 and 2), taking into account that the first of these variables affects the second in the classification of asthma severity as proposed in GEMA 2009.12 However, the detection of an inverse correlation, albeit weak, between the degree of compliance with the AAM received and the level of asthma control (see Table 2) is more unexpected. This finding, contrary to the initial hypothesis of this study, can certainly be interpreted in different ways: (a) more symptomatic patients make more of an effort to adopt appropriate allergen avoidance practices, (b) compliance with a greater percentage of AAM does not necessarily imply rigorous compliance with the most clinically relevant AAM and, consequently, the quantitative evaluation by which the degree of compliance with AAM received was classified in this study perhaps is not the most appropriate for evaluating the possible influence of this variable on the level of asthma control and (c) due to the characteristics of the study itself (i.e. a subjective method of identification of the AAM received and followed by the patients and physicians, respectively), the presence of some type of bias in the analysis of the relationship between these two variables cannot be definitively ruled out.
Nevertheless, there are some more issues worth considering regarding the AAM. Since the content of the AAM received by patients in the past may have been slightly different depending on the hospital where they were diagnosed, we tried to standardize the subjective medical evaluation of their compliance by presenting all physicians with the same questionnaire, as well as defining beforehand the criteria for determining if the various AAM were followed by the patients or not (see Patients and Methods). In this way, we managed to reduce the number of variables assessed in a truly “subjective” manner to only one: the number of AAM that the patients stated they had received (the AAM given by the physicians to their patients is not usually reflected in their medical records). Accordingly, we feel that we reduced the possibility that there was really an information bias, or at least that its magnitude was less.
In short, this study has shown that the real situation of patients with allergic asthma attending Spanish Respiratory Medicine departments, in relation to the allergic nature of their disease, is characterized by: (a) a suboptimal degree of knowledge of their allergies, (b) incomplete information received regarding the AAM that should be followed, (c) reasonably good compliance with these AAM by the majority of patients who received them, and (d) the existence of only one-third of patients who knew all of their allergies and who followed appropriate allergen avoidance practices.
These four findings are highly significant because, as mentioned above, as far as we are aware, until now none of them have been evaluated in previous publications. Extrapolating these findings to the overall allergic asthma population could be questionable for the following two reasons: (a) the patients studied here may represent a select group of patients with a considerably high education level, taking into account that 76% of them had middle or higher level studies and (b) these patients, having been attended by pulmonologists in hospital outpatient clinics, may have received more extensive and precise information about their allergic disease, compared to that which patients seen in other settings, such as primary care centers, may receive. However, even assuming that this may be the case, we think that the results presented here are still relevant, since they reflect inadequate management of the allergic component of the disease, and if they are biased, it would be reasonable to expect that the real situation is even more disappointing for patients with a lower educational level or who are not treated by specialists. In this respect, more studies in the primary care setting and in other specialist departments involved in the management of these patients, e.g. allergology units, might clarify whether our results can be extrapolated, to a greater or lesser extent, to the context of other medical settings.
Another two relevant aspects that may have influenced our results are the characteristics of the patient recruitment process and the manner of classifying the degree of patient knowledge of their allergic sensitizations and compliance with the AAM received by the patients. With regard to the first, it must be emphasized that this is a multicenter study, with inclusion of patients from different geographical regions and sociocultural settings, which in principle, should make the results more consistent. However, the inclusion period of nine months required to enroll 147 patients would suggest that some patients who were candidates for enrolment were not assessed. Even accepting that this could have occurred in any participating hospital, we do not think that this incurred a significant selection bias, for the following reasons: (a) the number of patients included in the various hospitals and provinces was reasonably homogeneous (see Patients and Methods) and (b) all of them were diagnosed in the setting of a hospital Respiratory Medicine outpatient clinic, and as such, a certain degree of homogeneity can be assumed with respect to clinical severity, therapeutic management and the patients’ knowledge of their disease.
With respect to the second aspect, the reason for the selection of the method for classification of the allergic sensitizations and the patients’ compliance with the AAM has already been discussed in the Patients and Methods section. In the absence of a previous description in the literature of other quantitative classification methods for these variables, our requirement that the patients knew all their allergic sensitizations or followed all the AAM received in order for their degree of knowledge of their allergies or their allergen avoidance practices to be considered “high” or “appropriate” may be thought too strict. Indeed, other criteria may have been equally valid, for example, a >75% compliance with the variable or equal to the mean+2 standard deviations. However, we understand that, just as the objective in the treatment of asthma must be the total control of all symptoms, the objectives in the two variables mentioned here must be 100% compliance. We also recognize that we could have set different cut-off points for establishing the various levels of compliance of these variables (zero, low, medium and high), but we do not feel that this would have yielded different results for the influence of both variables on the level of asthma control, taking into account, as discussed in the Patients and Methods section, that the percentage of compliance with both variables was sufficiently differentiated when it was done in this way.
In all, our results call into question the quality of the information and education received by our allergic asthma patients. As such, a greater effort must be made in education to improve patients’ knowledge of the allergic nature of their disease. With this aim, it would be appropriate to review the educational strategies and practices of our healthcare professionals and to analyze not only the way in which patients are instructed about allergen avoidance practices, but also about many other relevant educational aspects of their disease (importance of continued anti-inflammatory treatment, avoidance of irritants, self-management plans, etc.). Moreover, patient education methods should also be studied with the aim of identifying variables that could possibly increase knowledge of and adherence to the recommendations. Meantime, it seems advisable to incorporate systems for monitoring patients’ adherence to the standard clinical recommendations and for avoiding limiting the educational effort to the mere transmission of recommendations into routine clinical practice. Likewise, perhaps in the near future, the introduction of new technology in this field may be helpful for improving the knowledge and capabilities of our patients in managing their allergies.
Conflict of InterestThe authors declare no conflict of interest in relation to the content of the study.
Please cite this article as: Roger À, et al. Grado de conocimiento de las propias sensibilizaciones alérgicas en pacientes asmáticos y su repercusión en el nivel de control del asma. Arch Bronconeumol. 2013;49:289–96.