Malignant pleural effusion (MPE) is a medical problem commonly encountered in daily practice. Approximately one third of cases are associated with lung cancer, while the second most common cause is metastatic breast cancer.1
The therapeutic objective in MPE is relief of associated respiratory symptoms. The use of small-caliber tunneled indwelling pleural catheters (IPC) in an outpatient setting is a good option in the palliative care of MPE patients.2
Clinical CaseThis was a 64-year-old man with a smoking history of 47 pack-years.
He was diagnosed with stage IV lung adenocarcinoma in January 2013, and at that time he was receiving his first cycle of chemotherapy with carboplatin and paclitaxel.
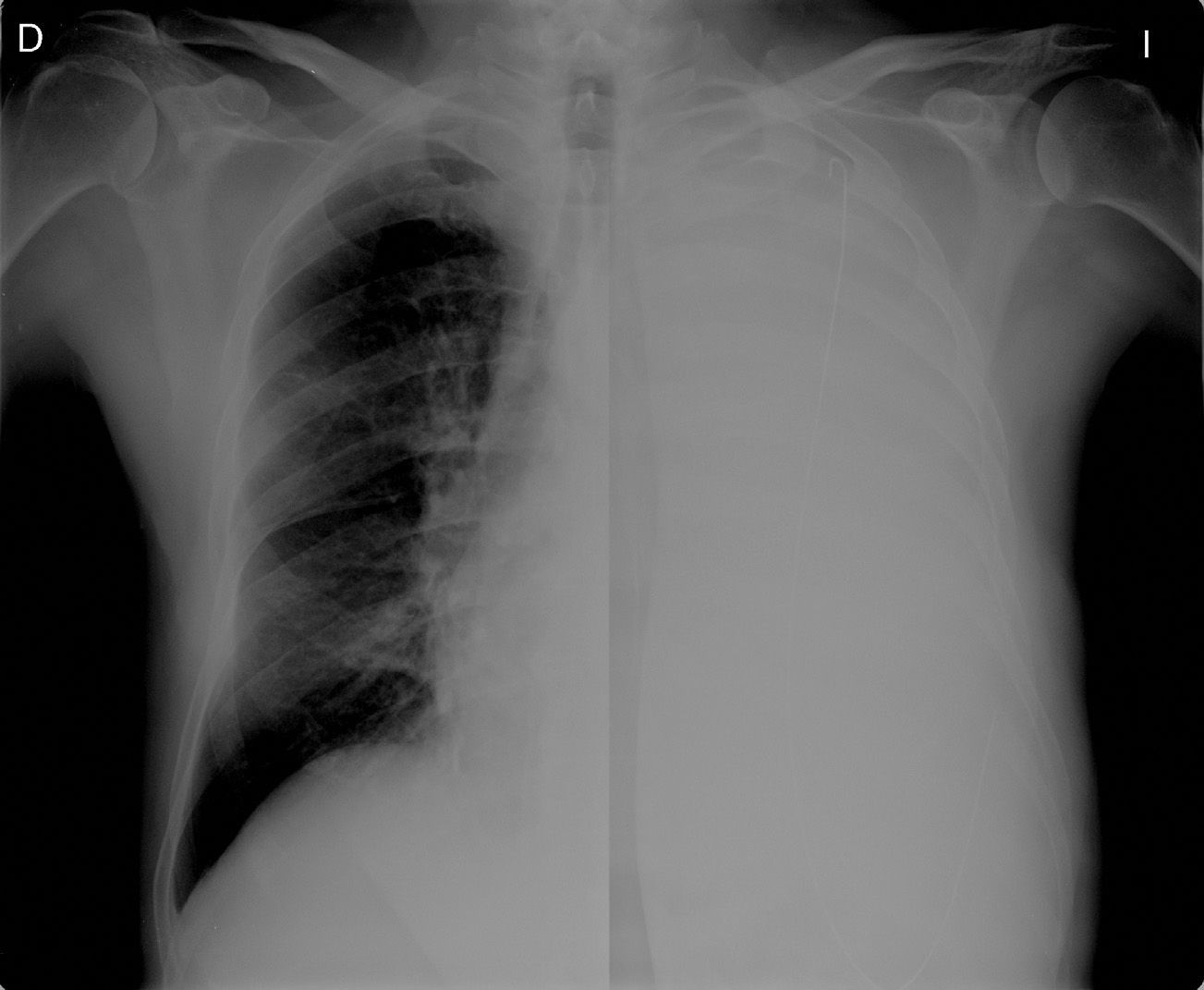
Imaging studies showed a pulmonary mass in the left upper lobe, lymphangitis with moderate left pleural effusion and pleural implants.
Cytology of pleural effusion fluid after thoracocentesis showed malignant cells in the pleural fluid.
In view of recurrent, symptomatic malignant pleural effusion (drained on 5 occasions), the decision was taken to place a Pleurx® IPC in the left hemithorax.
During the Pleurx® placement procedure, the metal guide-wire accidentally invaded the pleural cavity (Fig. 1).
DiscussionIn recent years, the use of IPC in the management of recurrent MPE has increased. Although the device is designed to remain permanently in situ, in certain patients (those with spontaneous pleurodesis), the IPC can be withdrawn when pleural effusion resolves. This device successfully controls symptoms in 95.4% of patients.2
Few complications associated with catheter placement and maintenance have been described, and any that do occur are easily managed. Solutions range from replacing the drainage tube during insertion to checking for spontaneous displacement, pleural fluid leakage and skin infections around the insertion site during monthly follow-up visits.3
The main complication of IPC is infection,4 the probability of which is 7.5%. With regard to infections, distinction should be made between pleural fluid infection (empyema) and skin infection. The risk of cellulitis-type skin infection is even lower than with other indwelling devices (hemodialysis/peritoneal dialysis catheters).3
In the most complete series published to date in Spain, Cases et al.2 described 63 patients who had received an IPC. Complications during follow-up included 3 cases with empyema, 2 cases of chest pain requiring catheter replacement and 3 cases of tumor dissemination around the tube insertion site.
In conclusion, serious or severe complications (requiring an additional invasive procedure or hospital admission) with IPEs are rare, and the device can be managed by the patient or by family members in the home.5
However, IPE placement involves a learning curve, and great care must be taken in the process of both insertion and removal.
Fortunately, in our case, the metal guide-wire could be removed without complications by performing a thoracoscopy. The procedure was completed with correct placement of the IPE.
Please cite this article as: Briones-Gómez A, Modesto-Alapont M, Muñoz-Moya MA, Martínez-Tomás R, Cases-Viedma E. Inserción de guía metálica en la cavidad pleural como complicación en la colocación de catéter de drenaje pleural permanente tunelizado. Arch Bronconeumol. 2015;51:206–207.