Health-related quality of life is an important outcome measurement in the monitoring of asthma control. Self-efficacy is a determinant of self-management behaviors that can contribute to the improvement of asthma control and quality of life. Our objective was to analyze the relationship between self-efficacy and quality of life in children with asthma and their caregivers.
MethodsWe included 176 patients aged 6–14 years with asthma, and determined their level of self-efficacy according to three groups (low, medium and high levels). Each child and their main caregiver completed the PAQLQ and PACQLQ questionnaires, respectively.
ResultsPAQLQ range=1–7: 5.61±1.11; PACQLQ range=1–7: 5.42±1.35; self-efficacy range=0–60: low level 28.44±4.58; average level 37.41±1.7, and high level 47.50±5.5. Significant differences were observed in quality of life according to low-medium vs high levels of self-efficacy. Specific related domains: PAQLQ emotions and PAQLQ symptoms with self-efficacy in problem-solving skills related to asthma and treatment self-efficacy; PACQLQ emotions with self-efficacy in problem-solving skills related to asthma.
ConclusionsA high level of self-efficacy is associated with a better quality of life for children and their caregivers. Based on these results, the measurement of self-efficacy could be incorporated in the assessment of educational interventions in self-management targeted at the quality of life of the patient and his or her family.
La calidad de vida relacionada con la salud es una importante medida de resultado utilizada en la monitorización del control del asma. La autoeficacia es un determinante de las conductas de automanejo, por lo que puede contribuir a la mejora del control del asma y de la calidad de vida. Nuestro objetivo es analizar la relación entre la autoeficacia y la calidad de vida de niños con asma y la de sus cuidadores.
MétodosEn un total de 176 pacientes entre 6-14 años con asma se ha determinado el nivel de autoeficacia identificando tres grupos (niveles bajo, medio y alto). Cada niño y su cuidador principal completan PAQLQ y PACQLQ, respectivamente.
ResultadosPAQLQ rang=(1-7): 5,61±1,11; PACQLQ rang=(1-7): 5,42±1,35; autoeficacia rang=(0-60): nivel bajo 28,44±4,58; nivel medio 37,41±1,7 y nivel alto 47,50±5,5. Diferencias significativas en calidad de vida según niveles de autoeficacia bajo-medio vs alto. Dominios específicos relacionados: PAQLQ emociones y PAQLQ síntomas con autoeficacia en las habilidades para resolver problemas relacionados con el asma y autoeficacia para el tratamiento. PACQLQ emociones con autoeficacia en las habilidades para resolver problemas relacionados con el asma.
ConclusionesUn alto nivel de autoeficacia se asocia a una mejor calidad de vida de los niños y sus cuidadores. Basándonos en estos resultados, la medida de la autoeficacia podría ser incorporada en la evaluación de las intervenciones educativas en automanejo cuyo objetivo final es alcanzar la calidad de vida diana del paciente y su familia.
Self-management is an effective way of achieving and maintaining asthma control, the main goal of treatment.1 This approach requires that the individual be empowered and that their needs and perceptions are given the necessary importance. As a result, conventional clinical outcome measures have been supplemented with other patient-centered variables (patient-reported outcomes measures [PROM]), an approach which has become increasingly common among pediatric patients in recent years.2
Health-related quality of life is an important PROM that is closely related with the degree of asthma control,3–5 and is a key element in the monitoring of the latter.6
Various studies have shown that quality of life is determined by many factors, although the results are less robust when objective criteria are used7–9 than when subjective parameters are taken into account.10,11 One of the most important subjective parameters is self-efficacy, defined as an individual's belief in their ability to successfully perform a behavior.
Self-efficacy plays a key role in the self-management of asthma,12 and has been included as a basic component in educational interventions aimed at achieving optimal quality of life in patients.13 Studies in adults have found associations between self-efficacy and patient quality of life.14–16 In the pediatric population, parental self-efficacy has also been associated with children's quality of life and other indicators of morbidity.17,18
However, in spite of the apparent importance of self-efficacy in quality of life, we still do not have sufficient data on this relationship from the perspective of the child.
The aim of this study, then, was to analyze the quality of life of children and caregivers according to the level of self-efficacy shown by the children in the management of their asthma.
MethodsThis was a descriptive, cross-sectional study conducted in a university hospital and primary care centers of reference in the Mar Menor area, in the southeast of Spain.
All pediatric outpatients and their caregivers who met the following criteria were included: (a) children between 6 and 14 years; (b) medical diagnosis of asthma; (c) good level of literacy in Spanish; (d) written consent.
The study was performed between November 2010 and December 2011. The research protocol was approved by the relevant ethics committees.
Self-efficacy was assessed using the adapted version of the Asthma Self-efficacy Scale validated in Spanish19 (Appendix A, Annex A, available in the electronic version). This scale assesses the beliefs of children about their ability to carry out certain self-management behaviors that are necessary for appropriate asthma control. It includes 20 items of which 19 are distributed in four domains: self-efficacy in skills for solving asthma-related problems (6 items), self-efficacy for treatment (6 items), self-efficacy in the doctor–patient relationship (4 items), and self-efficacy in solving interpersonal problems (3 items). Each item is answered on a Likert-type scale with four response options, where 0=not at all confident; 1=not very confident; 2=confident; 3=very confident. The final score is the sum of the responses in each item, providing an overall score and a specific score for each of the domains.
The Paediatric Asthma Quality of Life Questionnaire (PAQLQ)20–22 and the Paediatric Asthma Caregiver's Quality of Life Questionnaire (PACQLQ)23 were used to evaluate the quality of life of children and their caregivers, respectively (Appendix A, Annex B and C, available in the online version). The PAQLQ consists of 23 items structured in three domains: activity limitations (5 items), emotional function (8 items), and symptoms (10 items). For the activity limitation domain, the version of individualized items from the standardized list of activities was used.21,22 The PACQLQ consists of 13 items set out in two domains: emotional function (9 items) and activity limitation (4 items). The result of both questionnaires will be expressed in the form of a mean score that can range from 1 (maximum limitation) to 7 points (no limitation).
The children completed the tests during a personal interview conducted by a single trained examiner using a visual analog scale. The caregivers completed a self-administered form.
The distribution of the data indicated the use of non-parametric tests. The Kruskal–Wallis test was used to compare quality of life scores among the 3 patient groups (low, medium, and high levels of self-efficacy) obtained by tertiles. Possible differences between 2 groups were evaluated using the Mann–Whitney U test. Statistical significance was set at a P-value of less than 0.05 in all tests.
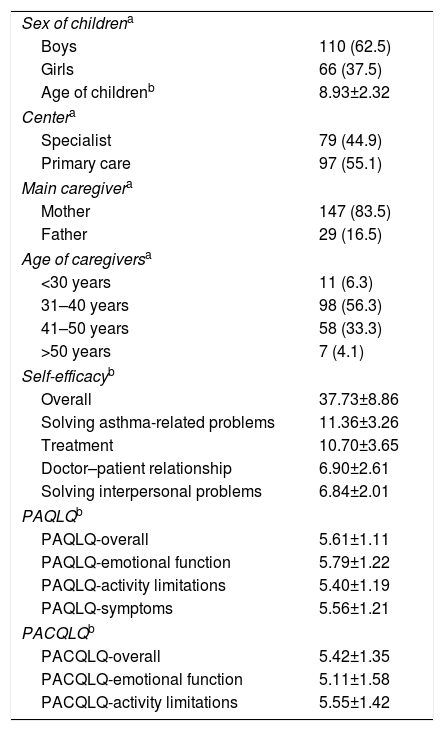
ResultsA total of 217 eligible patients were identified, although 41 were excluded (35 could not be located, 4 refused to participate, and 2 lacked the required language skills). The final sample comprised 176 children and their caregivers. Cohort characteristics are shown in Table 1. We observed a greater proportion of male patients (62.5%), and more mothers (83.5%) were the main caregiver.
Study Population.
| Sex of childrena | |
| Boys | 110 (62.5) |
| Girls | 66 (37.5) |
| Age of childrenb | 8.93±2.32 |
| Centera | |
| Specialist | 79 (44.9) |
| Primary care | 97 (55.1) |
| Main caregivera | |
| Mother | 147 (83.5) |
| Father | 29 (16.5) |
| Age of caregiversa | |
| <30 years | 11 (6.3) |
| 31–40 years | 98 (56.3) |
| 41–50 years | 58 (33.3) |
| >50 years | 7 (4.1) |
| Self-efficacyb | |
| Overall | 37.73±8.86 |
| Solving asthma-related problems | 11.36±3.26 |
| Treatment | 10.70±3.65 |
| Doctor–patient relationship | 6.90±2.61 |
| Solving interpersonal problems | 6.84±2.01 |
| PAQLQb | |
| PAQLQ-overall | 5.61±1.11 |
| PAQLQ-emotional function | 5.79±1.22 |
| PAQLQ-activity limitations | 5.40±1.19 |
| PAQLQ-symptoms | 5.56±1.21 |
| PACQLQb | |
| PACQLQ-overall | 5.42±1.35 |
| PACQLQ-emotional function | 5.11±1.58 |
| PACQLQ-activity limitations | 5.55±1.42 |
According to the results in the self-efficacy scale, only 37.9% of the children stated that they were confident/very confident with their ability to manage their asthma. In the self-efficacy domains, 48.9% were confident/very confident with their skills in solving asthma-related problems, 42.7% with their self-efficacy in solving interpersonal problems, and 39.2% with their doctor–patient relationship. Self-efficacy for solving interpersonal problems, reported by 73.9% of subjects, was the domain in which the children considered themselves most competent.
With regard to quality of life, 95.5% of the children were found to have some degree of limitation as a result of their asthma, with scores of less than 7 on the overall PAQLQ (a score of 7 indicates no limitation). The percentage of subjects affected in the PAQLQ domains of activity limitation, emotional function, and symptoms was 87.5%, 84.7% and 92%, respectively. The activities of the list that generated most limitation were running (92 choices) and playing football (53 choices). The quality of life of caregivers was also altered, with a score of less than 7 in 86.4% of the cases according to overall PACQLQ score, 77.3% in the activity limitation domain, and 82.4% in the emotional function domain.
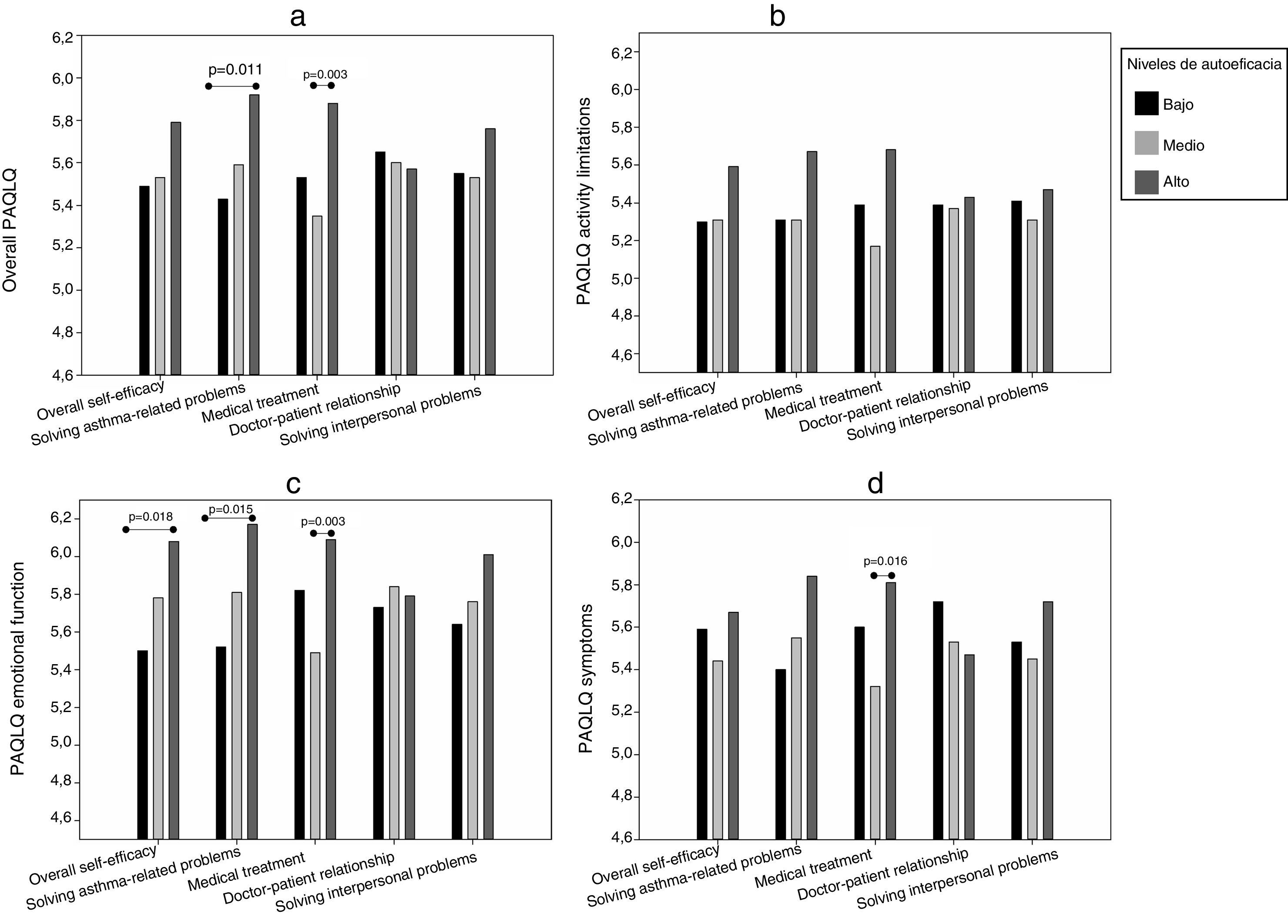
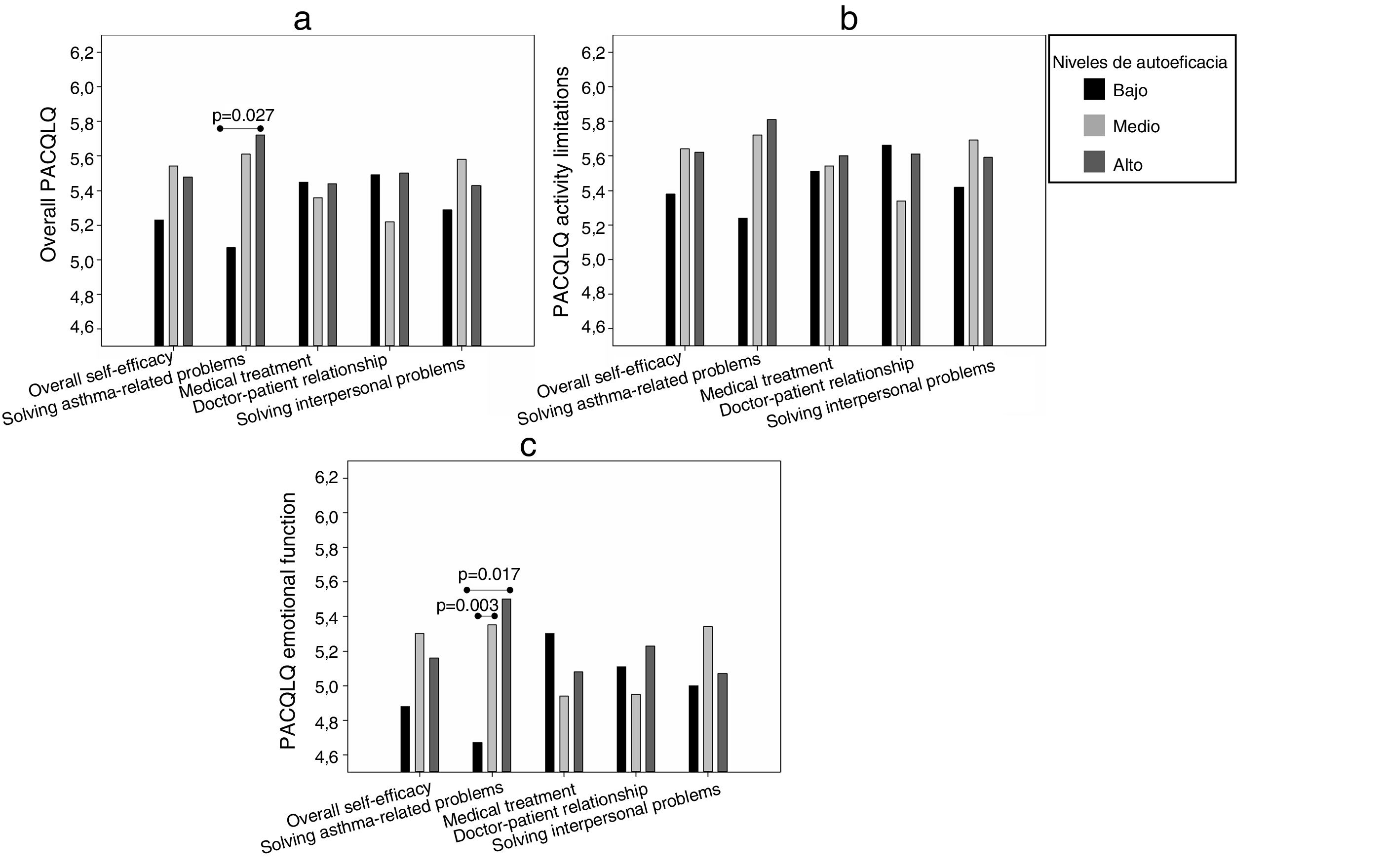
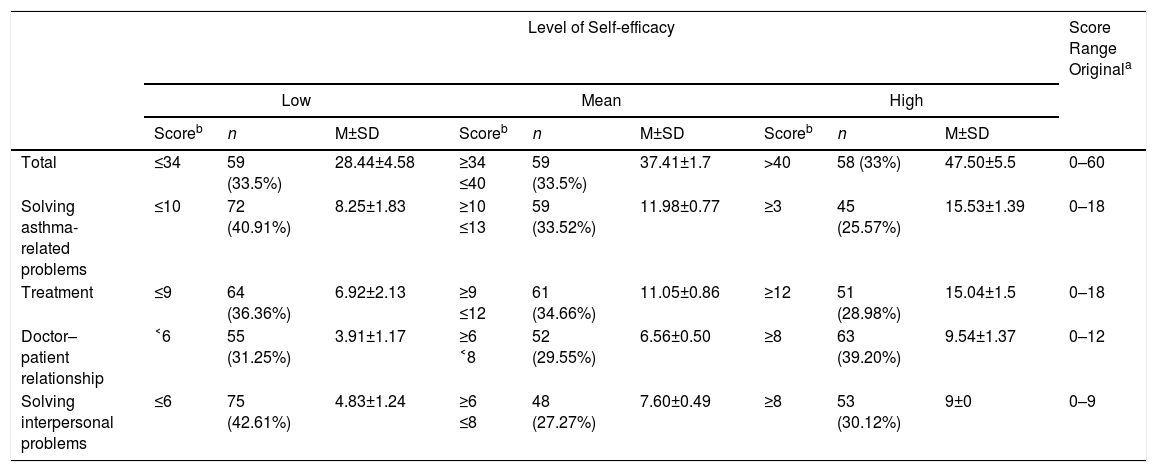
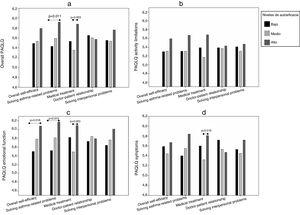
To analyze quality of life associated with self-efficacy, we identified three groups of patients with different levels of self-efficacy (low, medium and high) for the total scale and its dimensions. Table 2 shows the cut-off score that defined each group, its size, and average scores. It was observed that, in most domains, the high self-efficacy group presented higher mean quality of life scores, among both children (Fig. 1) and their caregivers (Fig. 2), although the results of the analysis of the other dimensions were not significant.
Level of Self-efficacy: Mean Score and Size of the Groups According to Cut-off Score.
| Level of Self-efficacy | Score Range Originala | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low | Mean | High | ||||||||
| Scoreb | n | M±SD | Scoreb | n | M±SD | Scoreb | n | M±SD | ||
| Total | ≤34 | 59 (33.5%) | 28.44±4.58 | ≥34 ≤40 | 59 (33.5%) | 37.41±1.7 | >40 | 58 (33%) | 47.50±5.5 | 0–60 |
| Solving asthma-related problems | ≤10 | 72 (40.91%) | 8.25±1.83 | ≥10 ≤13 | 59 (33.52%) | 11.98±0.77 | ≥3 | 45 (25.57%) | 15.53±1.39 | 0–18 |
| Treatment | ≤9 | 64 (36.36%) | 6.92±2.13 | ≥9 ≤12 | 61 (34.66%) | 11.05±0.86 | ≥12 | 51 (28.98%) | 15.04±1.5 | 0–18 |
| Doctor–patient relationship | ˂6 | 55 (31.25%) | 3.91±1.17 | ≥6 ˂8 | 52 (29.55%) | 6.56±0.50 | ≥8 | 63 (39.20%) | 9.54±1.37 | 0–12 |
| Solving interpersonal problems | ≤6 | 75 (42.61%) | 4.83±1.24 | ≥6 ≤8 | 48 (27.27%) | 7.60±0.49 | ≥8 | 53 (30.12%) | 9±0 | 0–9 |
In children, the overall PAQLQ results (Fig. 1a) were significant for the domains of self-efficacy in skills for solving asthma-related problems (P=0.044) and self-efficacy for treatment (P=0.012). With regard to the specific PAQLQ domains, activity limitations (Fig. 1b) showed no relationship with self-efficacy, although the result of the self-efficacy for treatment domain was almost significant (P=0.053). The PAQLQ emotional function domain (Fig. 1c) was the most closely related with the level of self-efficacy in the domains of skills for solving asthma-related problems (P=0.013) and treatment (P=0.008), as well as with overall self-efficacy (P=0.042); in the self-efficacy in solving interpersonal problems domain, the analysis seemed to indicate some kind of relationship, but statistical significance was not reached (P=0.060). The results for the PAQLQ symptoms domain (Fig. 1d) also showed a significant relationship with self-efficacy for treatment (P=0.049).
When quality of life (overall PAQLQ and PAQLQ emotional function) was compared by level of self-efficacy in skills for solving asthma-related problems and the level of overall self-efficacy, significant differences were found between the high and low levels (Fig. 1a and c), while in the domains of quality of life associated with self-efficacy for treatment, differences were found between the middle and high level (Fig. 1a, c and d).
In caregivers, overall PAQLQ results (Fig. 2a) indicated a significant association with the domain of self-efficacy in skills for solving asthma-related problems (P=0.046). The activity limitations domain (Fig. 2b) showed no significant association with self-efficacy, although the association between PACQLQ emotional function (Fig. 2c) and self-efficacy in skills for solving asthma-related problems was significant (P=0.026).
When mean overall PAQLQ was analyzed according to the level of self-efficacy in skills for solving asthma-related problems (Fig. 2a), significant differences were found between the low and high levels. In the PACQLQ emotional function domain, differences in quality of life were significant when the low level was compared with the medium and high levels (Fig. 2c).
DiscussionAsthma has a significant impact on quality of life, causing limitations in around 90% of the children and caregivers in our study. This high percentage may be an indicator of uncontrolled asthma in cases with PAQLQ scores lower than 6.2, the cut-off point established by Nordlund et al.24 as discriminatory for a lack of asthma control. In our series, 63.1% of children had this score (46.6% low to medium level of self-efficacy vs 16.5% high level; P=0.0001; data not shown). Severity is another factor that can explain the impact of asthma, especially on caregivers, since the greater the child's severity, the worse the caregiver's quality of life.7
However, quality of life is determined by multiple factors and as the results of this study show, self-efficacy plays a relevant role.
Although it is common to find high self-efficacy in children with asthma,25–27 in our study, 40% of our patients stated that they felt confident or very confident with their ability to manage asthma. Self-efficacy is not an isolated, static process, but a mechanism in which different levels and domains can be identified.19 We too perceived this specific characteristic in our study, as only two of its dimensions were associated with quality of life.
In the case of children, the PAQLQ activity limitations domain was the most affected, with results that are consistent with those obtained by other authors.21,22,24,28,29
In the list of standardized activities, most of our children reported the greatest limitation in activities such as running and playing football, findings that are also echoed in the literature.30 This limitation may be due to a lack of asthma control, since symptoms and frequent exacerbations prevent children from performing activities such as attending school, doing sports, or sleeping normally.4,31 Moreover, mistaken beliefs about exercise in children with asthma can cause many caregivers to be overprotective and to restrict the practice of an activity, and can even lead children themselves to avoid such activities.32 Although children with a high level of self-efficacy for treatment have fewer limitations, differences with the other groups were not significant.
The best results were obtained for the PAQLQ emotional function, the domain that has been shown to be clearly related to self-efficacy. High confidence in their skills for solving asthma-related problems, such as knowing if an exacerbation might worsen or avoiding triggers, has a positive effect on the patient's emotional state, a fact that has already been demonstrated in studies conducted in adults.33
A high level of self-efficacy for treatment also has a great impact on children's quality of life. The findings for PAQLQ emotional function and PAQLQ symptoms show that children with more self-efficacy have the best quality of life, although those who lack confidence in their ability to make decisions about medications and their administration have a better quality of life than those with an average level of self-efficacy. These results could be due to characteristics related to the development of self-efficacy in this domain, since one of the main sources of confidence is experience. Initially, the responsibility of caring for children with asthma is assumed by the caregivers, and subsequently transferred to the child.34 It is possible that the children in our study with low self-efficacy for treatment have not yet had the opportunity to make decisions regarding their medication, and lack confidence in their ability to manage it, but they are possibly confident that their caregivers are able to do so, conferring a higher emotional quality of life and reducing the impact of symptoms; while those who have a medium level of self-efficacy are still developing these skills, with the consequent effect on their well-being.
With regard to caregivers, our results are similar to those reported in other series.7,11,35,36 In our study, the most limited domain on the PACQLQ was emotional function, although self-efficacy in skills for asthma-related problems mitigates this impact. In this respect, continuous monitoring of a child may lead to a lack of independence for both child and caregiver, with negative consequences for the child's psychosocial development and the caregiver's quality of life. Children who are confident in their ability to identify and manage asthma-related problems, many of which can occur at times that their caregiver is absent, may feel less concerned and/or frustrated.
This is the first study published in our setting that examines the relationship between self-efficacy and quality of life in the pediatric population with asthma, taking the original approach of considering this analysis from the children's perspective, evaluating the impact of their own self-efficacy. The study sample comprised of children and caregivers also provides a more complete picture of the impact of the disease and reaffirms the ability of children to report on their own health.37–39
Our findings underline the importance of self-efficacy in the self-management of asthma, and have important applications in terms of clinical research and practice. The measurement of self-efficacy helps detect at-risk patients who require intervention to improve their quality of life. We therefore propose that self-efficacy be incorporated as a component of educational interventions designed to achieve the optimal quality of life of patient and their families.
Despite these advantages, our study also has some limitations. In addition to the difficulties associated with the use of PROM,2,40 the use of the PAQLQ in children aged 6 years could introduce bias. Some authors have reported problems using the instrument in children under 7 years of age,22,28 but in our study we resolved this by having an experienced interviewer administer the test, using a visual analog scale to support responses. In addition, we could not establish causal relationships between the variables due to the cross-sectional design of the study, so we recommend that future longitudinal studies are undertaken that include other determinants of quality of life that might affect the stability of the relationships found.
Nevertheless, we believe that the level of self-efficacy of children can mitigate the impact of asthma on their quality of life and that of their caregivers. Confidence in their ability to manage asthma improves children's perception of well-being and eases the burden of the caregiver, resulting in an improved quality of life for both.
In conclusion, a high level of self-efficacy is associated with a better quality of life among children and their caregivers. Based on these results, the measurement of self-efficacy could be incorporated in the assessment of educational interventions in self-management.
Conflict of InterestsThe authors state that they have no conflict of interests.
The authors are grateful for the help of the staff of the pediatric pulmonology unit of the Hospital Universitario Los Arcos del Mar Menor and thank all children and caregivers who participated for their interest in this study.
Please cite this article as: Melgarejo González-Conde V, Pérez-Fernández V, Ruiz-Esteban C, Valverde-Molina J. Impacto de la autoeficacia en la calidad de vida de niños con asma y sus cuidadores. Arch Bronconeumol. 2019;55:189–194.