Pulmonary hypertension (PH) secondary to respiratory conditions (group 3) is the second most frequent cause of PH after left-sided heart diseases, and it is more frequent the more advanced the disease is.1 Lung transplantation (LT) is a treatment option for patients with advanced chronic respiratory diseases. Therefore, a high percentage of patients who are candidates for LT have PH.2
The recent 2022 ESC/ERS guidelines have redefined group 3 PH as a mean pulmonary artery pressure (mPAP) >20mmHg measured by right heart catheterization (RHC) with a pulmonary vascular resistance (PVR) >2 Wood units. In contrast, the previous guidelines defined PH as mPAP >25 and PVR >3 Wood units.3 In addition, the recent 2022 document has changed the definition of severe group 3 PH: in the 2015 version, severe group 3 PH was defined as a mPAP >35mmHg and/or a mPAP ≥25mmHg and a cardiac index <2.5l/min/m2, while the current version has defined severe group 3 PH as a mPAP >20mmHg and PVR >5 Wood units. Finally, the 2022 guideline provides a new concept of unclassified PH, defined as mPAP >20mmHg but with PVR <2 Wood units.
The main objective of this study is to evaluate the impact of the change in the definition of PH and severe PH in group 3 in a cohort of patients with severe respiratory disease included on the waiting list for LT, and whether this change in definition has an impact in the postoperative outcomes, mainly primary graft dysfunction (PGD).
A retrospective study was carried out including patients with advanced respiratory diseases included on the waiting list for LT at the Marqués de Valdecilla University Hospital in Santander between 03/01/2014 and 10/31/2022. Severe PH was defined according to the 2015 guidelines as mPAP >35mmHg or mPAP ≥25mmHg with a cardiac index <2.5l/min/m2, and according to the 2022 guidelines as a PAPm >20mmHg and PVR >5 Wood units. In addition, unclassified PH was defined as mPAP >20mmHg with PVR <2 Wood units. Since 01/01/2019, all patients at our institution are studied with RHC in the pre-transplant study. Before that date, patients under 40 years of age and without signs of PH on the echocardiogram were not studied with RHC. These patients were predominantly cystic fibrosis. Characteristics of the patients at the time of inclusion on the waiting list and the immediate post-transplant period were collected. PGD was defined according to the ISHLT criteria.4 Statistical analysis was performed with the IBM SPSS Statistics 20 software package. Univariate logistic regression analysis to predict the risk of PGD was performed to estimate the odds ratio (OR) and 95% confidence interval (CI). A p value of 0.05 was considered statistically significant.
380 patients were included on the waiting list for LT, 94 patients were excluded from the study for several reasons: 29 not having pre-transplant catheterization, 2 re-transplantation, 24 due to respiratory pathologies different than group 3 PH (6 Langerhans histiocytosis, 2 sarcoidosis and 16 PAH group 1), and another 39 patients who did not have all the hemodynamic variables needed to define the study entities. The time elapsed from RHC to inclusion on the waiting list was 2.2 (0.93–5.83) months.
Finally, 286 patients were analyzed. According to the 2015 classification, 50.7% had PH and among these, 60.7% met the criteria for severe PH. According to the 2022 classification, 58% of patients had PH, but only 8.4% were severe PH, and 15.4% met the criteria for unclassified PH (73.4% of PH in total).
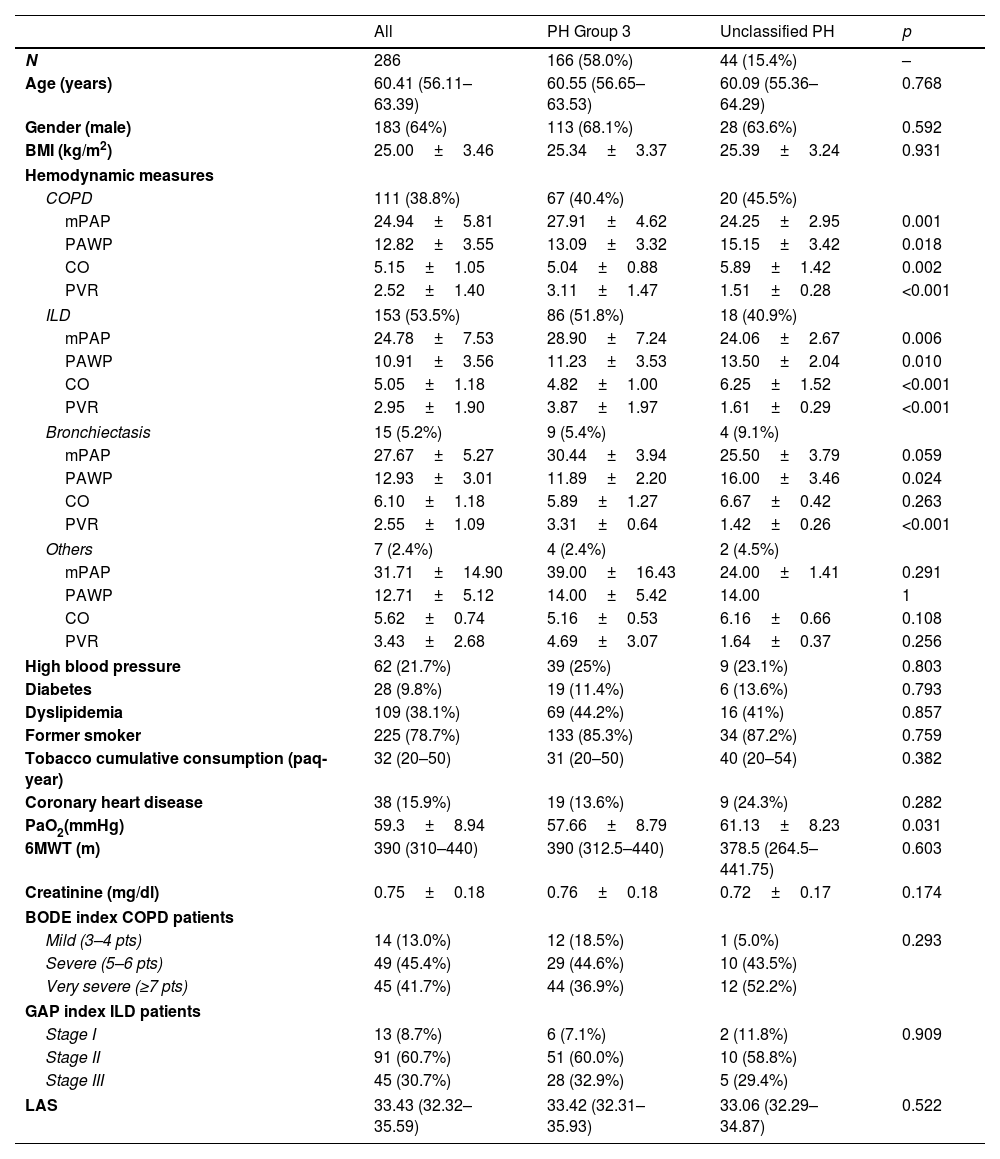
In compliance with the 2022 guidelines, no significant differences were found in any of the baseline characteristics between group 3 PH and unclassified PH, except in PaO2, which was slightly higher in unclassified PH (Table 1). In some cases the PAWP is in the limit values of 15mmHg. However, it is necessary to take into account that these are patients with advanced respiratory disease in whom making a precise measurement of this measure is complicated by respiratory variations.
Baseline Characteristics of Patients Included on the Waiting List for Lung Transplantation.
| All | PH Group 3 | Unclassified PH | p | |
|---|---|---|---|---|
| N | 286 | 166 (58.0%) | 44 (15.4%) | – |
| Age (years) | 60.41 (56.11–63.39) | 60.55 (56.65–63.53) | 60.09 (55.36–64.29) | 0.768 |
| Gender (male) | 183 (64%) | 113 (68.1%) | 28 (63.6%) | 0.592 |
| BMI (kg/m2) | 25.00±3.46 | 25.34±3.37 | 25.39±3.24 | 0.931 |
| Hemodynamic measures | ||||
| COPD | 111 (38.8%) | 67 (40.4%) | 20 (45.5%) | |
| mPAP | 24.94±5.81 | 27.91±4.62 | 24.25±2.95 | 0.001 |
| PAWP | 12.82±3.55 | 13.09±3.32 | 15.15±3.42 | 0.018 |
| CO | 5.15±1.05 | 5.04±0.88 | 5.89±1.42 | 0.002 |
| PVR | 2.52±1.40 | 3.11±1.47 | 1.51±0.28 | <0.001 |
| ILD | 153 (53.5%) | 86 (51.8%) | 18 (40.9%) | |
| mPAP | 24.78±7.53 | 28.90±7.24 | 24.06±2.67 | 0.006 |
| PAWP | 10.91±3.56 | 11.23±3.53 | 13.50±2.04 | 0.010 |
| CO | 5.05±1.18 | 4.82±1.00 | 6.25±1.52 | <0.001 |
| PVR | 2.95±1.90 | 3.87±1.97 | 1.61±0.29 | <0.001 |
| Bronchiectasis | 15 (5.2%) | 9 (5.4%) | 4 (9.1%) | |
| mPAP | 27.67±5.27 | 30.44±3.94 | 25.50±3.79 | 0.059 |
| PAWP | 12.93±3.01 | 11.89±2.20 | 16.00±3.46 | 0.024 |
| CO | 6.10±1.18 | 5.89±1.27 | 6.67±0.42 | 0.263 |
| PVR | 2.55±1.09 | 3.31±0.64 | 1.42±0.26 | <0.001 |
| Others | 7 (2.4%) | 4 (2.4%) | 2 (4.5%) | |
| mPAP | 31.71±14.90 | 39.00±16.43 | 24.00±1.41 | 0.291 |
| PAWP | 12.71±5.12 | 14.00±5.42 | 14.00 | 1 |
| CO | 5.62±0.74 | 5.16±0.53 | 6.16±0.66 | 0.108 |
| PVR | 3.43±2.68 | 4.69±3.07 | 1.64±0.37 | 0.256 |
| High blood pressure | 62 (21.7%) | 39 (25%) | 9 (23.1%) | 0.803 |
| Diabetes | 28 (9.8%) | 19 (11.4%) | 6 (13.6%) | 0.793 |
| Dyslipidemia | 109 (38.1%) | 69 (44.2%) | 16 (41%) | 0.857 |
| Former smoker | 225 (78.7%) | 133 (85.3%) | 34 (87.2%) | 0.759 |
| Tobacco cumulative consumption (paq-year) | 32 (20–50) | 31 (20–50) | 40 (20–54) | 0.382 |
| Coronary heart disease | 38 (15.9%) | 19 (13.6%) | 9 (24.3%) | 0.282 |
| PaO2(mmHg) | 59.3±8.94 | 57.66±8.79 | 61.13±8.23 | 0.031 |
| 6MWT (m) | 390 (310–440) | 390 (312.5–440) | 378.5 (264.5–441.75) | 0.603 |
| Creatinine (mg/dl) | 0.75±0.18 | 0.76±0.18 | 0.72±0.17 | 0.174 |
| BODE index COPD patients | ||||
| Mild (3–4 pts) | 14 (13.0%) | 12 (18.5%) | 1 (5.0%) | 0.293 |
| Severe (5–6 pts) | 49 (45.4%) | 29 (44.6%) | 10 (43.5%) | |
| Very severe (≥7 pts) | 45 (41.7%) | 44 (36.9%) | 12 (52.2%) | |
| GAP index ILD patients | ||||
| Stage I | 13 (8.7%) | 6 (7.1%) | 2 (11.8%) | 0.909 |
| Stage II | 91 (60.7%) | 51 (60.0%) | 10 (58.8%) | |
| Stage III | 45 (30.7%) | 28 (32.9%) | 5 (29.4%) | |
| LAS | 33.43 (32.32–35.59) | 33.42 (32.31–35.93) | 33.06 (32.29–34.87) | 0.522 |
BMI: body mass index; COPD: chronic obstructive pulmonary disease; ILD: interstitial lung disease; mPAP: mean pulmonary artery pressure; PAWP: pulmonary arterial wedge pressure; CO: cardiac output; PVR: pulmonary vascular resistance; 6MWT: 6min walking test; LAS: lung allocation score.
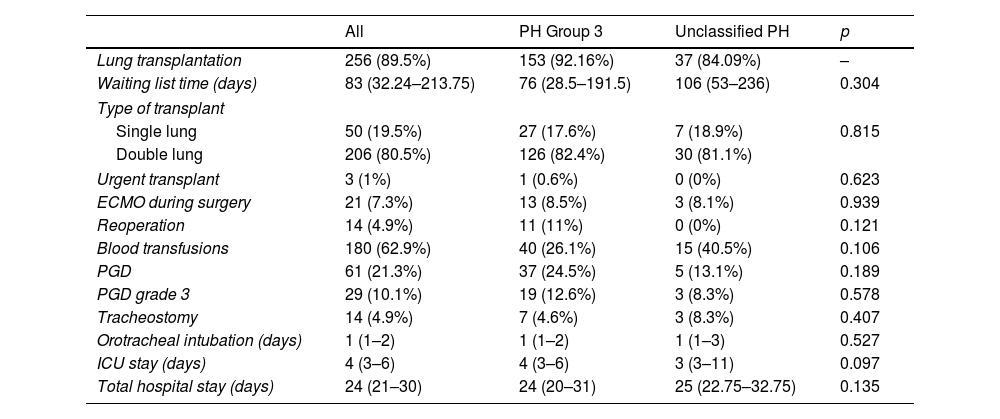
Of the 286 patients analyzed, 256 (89.5%) were transplanted in that period. No significant differences were found in any of the variables studied, neither in the time on the waiting list, nor in the need for an urgent transplant, use of ECMO during surgery, need for transfusions during surgery, need for reinterventions surgical procedures, primary graft dysfunction, intubation time, length of stay in the ICU or length of hospital stay between group 3 PH and unclassifiable PH (Table 2).
Outcomes After Lung Transplantation.
| All | PH Group 3 | Unclassified PH | p | |
|---|---|---|---|---|
| Lung transplantation | 256 (89.5%) | 153 (92.16%) | 37 (84.09%) | – |
| Waiting list time (days) | 83 (32.24–213.75) | 76 (28.5–191.5) | 106 (53–236) | 0.304 |
| Type of transplant | ||||
| Single lung | 50 (19.5%) | 27 (17.6%) | 7 (18.9%) | 0.815 |
| Double lung | 206 (80.5%) | 126 (82.4%) | 30 (81.1%) | |
| Urgent transplant | 3 (1%) | 1 (0.6%) | 0 (0%) | 0.623 |
| ECMO during surgery | 21 (7.3%) | 13 (8.5%) | 3 (8.1%) | 0.939 |
| Reoperation | 14 (4.9%) | 11 (11%) | 0 (0%) | 0.121 |
| Blood transfusions | 180 (62.9%) | 40 (26.1%) | 15 (40.5%) | 0.106 |
| PGD | 61 (21.3%) | 37 (24.5%) | 5 (13.1%) | 0.189 |
| PGD grade 3 | 29 (10.1%) | 19 (12.6%) | 3 (8.3%) | 0.578 |
| Tracheostomy | 14 (4.9%) | 7 (4.6%) | 3 (8.3%) | 0.407 |
| Orotracheal intubation (days) | 1 (1–2) | 1 (1–2) | 1 (1–3) | 0.527 |
| ICU stay (days) | 4 (3–6) | 4 (3–6) | 3 (3–11) | 0.097 |
| Total hospital stay (days) | 24 (21–30) | 24 (20–31) | 25 (22.75–32.75) | 0.135 |
PGD: primary graft dysfunction; ICU: intensive care unit.
Using the 2015 classification, in the univariate analysis, the presence of PH was not a risk factor for PGD (OR=1.142; 95% CI: 0.641–2.035; p=0.651) or PGD grade 3 (OR=1.934; 95% CI: 0.861–4.345; p=0.110), and severe PH was also not found to be a risk factor for PGD (OR=2.000; 95% CI: 0.899–4.448; p=0.089) nor PGD grade 3 (OR=1.479; 95% CI: 0.556–3.935; p=0.434).
Using the 2022 classification, in the univariate analysis, the presence of PH was not a risk factor for the PGD (OR=1.068; 95% CI: 0.593–1.924; p=0.826) or for PGD grade 3 (OR=1.324; 95% CI: 0.589–2.979; p=0.110), and severe PH was also not found to be a risk factor for PGD (OR=0.535; 95% CI: 0.113–2.533; p=0.430) nor for PGD grade 3 (OR=0.556; 95% CI: 0.068–5.534; p=0.583).
Although the results are interesting and show important changes, they must be interpreted with caution: first, it is a retrospective study, carried out in a single center. In addition, it is a selection of patients with severe respiratory disease included on the transplant waiting list, which does not represent the majority of patients with chronic respiratory diseases. Some studies have found an association between the presence of pre-transplant PH and the risk of PGD, but other series have not found similar results. This is a single experience, but future multicenter and prospective studies are needed to assess whether the new PH classification is useful in the prediction of PGD.
Therefore, with the new 2022 definition of PH group 3 compared to the 2015 definition, there is a marked increase in patients with PH criteria among patients with advanced respiratory disease, but with a lower frequency of severe PH. Moreover, despite the different definitions of group 3 PH and unclassified PH, no significant differences were found at baseline or in the immediate post-transplant follow-up. Thus, this new classification does not seem to be useful at the moment, at least in our patient cohort, differentiating between different groups of patients with advanced respiratory diseases, and it will be necessary to see in the future whether this differentiation between group 3 PH and unclassified PH it has diagnostic and/or prognostic utility.
Similarly, no differences in PGD risk were found between group 3 PH and group 3 severe PH between the 2015 and 2022 definitions. Although this new classification identifies more patients with PH but fewer patients with severe PH, it does not seem, at least as far as lung transplantation is concerned, to have prognostic implications in the appearance of PGD.
FundingThis research did not receive any fund from any public, private or non-profit entity.
Conflict of InterestThe authors declare no conflict of interest.