Hypersensitivity pneumonitis (HP) is a heterogeneous interstitial lung disease resulting from repeated exposure to organic or inorganic antigens. While rare in the pediatric population, with an estimated prevalence of 4 cases per million children,1 common triggers in children include bird antigens, fungal aerosols, and certain drugs. HP manifests as acute, sub-acute, or chronic forms, diagnosed based on (1) documented antigen exposure, (2) compatible respiratory symptoms, (3) decreased carbon monoxide transfer factor or exertional hypoxia, (4) specific radiologic features, and (5) lymphocytic alveolitis.2 Treatment involves antigen avoidance and occasionally corticosteroids. Here, we present a case of a 5-year-old girl diagnosed with HP due to exposure to turtledove droppings.
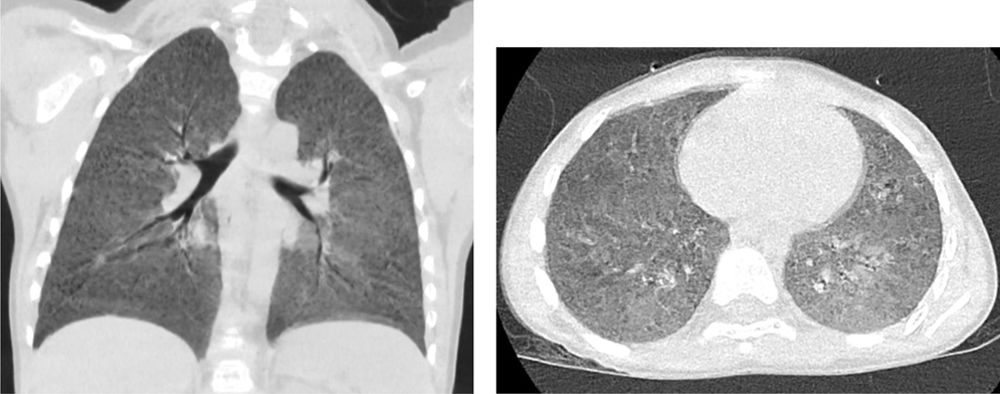
A 5-year-old girl was referred to our tertiary hospital for “recurrent asthma attack” with hypoxemia requiring three hospitalizations in one month. She had no prior history of asthma or atopy, either personally or in her family. She had experienced dyspnea and a dry cough for two months, accompanied by fever for one day at symptom onset and anorexia. On admission, she had tachypnea (57/min) with saturation at 88% in room air, needing supplemental oxygen. Chest auscultation was normal. Chest X-ray showed fine reticulation and diffuse opacities. A detailed environmental history revealed prolonged exposure to domestic turtledove (6 months), with excreta all over the apartment. Her respiratory signs were improved during hospitalization with steroid treatment but worsened upon each discharged at home. CT scan showed diffuse centro-lobular ground glass opacities (Fig. 1). Broncho-alveolar lavage (BAL) confirmed lymphocytic alveolitis with 1500cells/mm3 including 30% lymphocytes (normal range: <10%). The CD4/CD8 ratio was reversed (0.6; normal range: 0.9–2.5). Serum precipitin tests were positive for avian serum (IgG pigeon 91mgA/L, IgG chicken 32mgA/L; normal range<30, FEIA method), corroborated by the presence of specific arch (bird fancier's). Other causes of interstitial lung disease were ruled out through BAL studies, immunological assessments, and infectious disease screenings.
The patient was treated with 24h of oxygen and oral prednisone at 1mg/kg/day with tapering for a total of 3 months. Upon discharge with avoidance advice, the patient showed excellent evolution during follow-up. Her apartment was cleaned, and the bird was removed. After three months of steroid treatment, she had no more dyspnea, oxygen pulse oximetry was 99%, and she gained weight. Lung volume and DLCO was not possible because of her age.
HP is often underrecognized by pediatricians, leading to delayed diagnosis averaging between 1 and 11 months,2 with the risk of irreversible pulmonary fibrosis. Clinical recognition relies on exposure history and respiratory findings. Predominant pediatric triggers include bird or fungal antigens.3 Our case highlights HP in a 5-year-old exposed to domestic turtledove droppings, with only one similar case reported.4 Despite pigeons being more commonly cited, the allergens are common to both species, as they belong to the same taxonomic family, Columbidae.5 This case underlines the importance of environmental exposure interrogation in front of interstitial lung disease, for accurate diagnosis and treatment.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributions- -
Maggiolino Quentin: Conception and writing of the article. Bibliography collection.
- -
Socchi Floriane: Critical revision of the article.
- -
Renoux Marie-Catherine: Final approval of the article.
The authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.
Artificial intelligence involvementNo material in this manuscript has been produced with the help of any artificial intelligence software or tool.