We read with interest the case of a 33-year-old man with hemoptysis reported by Peghini Gavilanes et al.,1 in which contrast-enhanced computed tomography (CT) of the chest demonstrated a Rasmussen aneurysm secondary to tuberculous infection. The patient died 2 days later due to massive hemoptysis. Although Rasmussen aneurysms frequently present as nodular lesions within or adjacent to cavitary tuberculous lesions,1,2 they also may occur inside consolidations, making their identification more difficult.
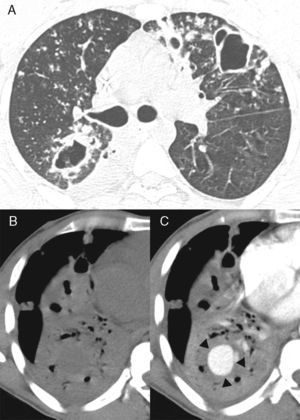
We would like to report a similar case of a 37-year-old man who was admitted to the emergency room with hemoptysis. The patient had a history of pulmonary tuberculosis (TB), treated irregularly for the previous 2 years. Sputum was positive for acid-fast bacilli. Fiberoptic bronchoscopy showed active bleeding from the right lower-lobe bronchus. Contrast-enhanced chest CT revealed nodules and cavities suggestive of active pulmonary TB, and consolidation in the right lower lobe with a rounded enhancing lesion within the consolidated area (Fig. 1). Transcatheter embolization with coils was performed. The patient also received TB therapy and recovered well, with no recurrence of bleeding during 1 year of follow-up.
(A) Axial CT image obtained with the lung window setting at the level of bronchial bifurcation, showing multiple bilateral nodules and cavities in the lung parenchyma. CT images obtained with the mediastinal window setting at the level of the lower lobes before (B) and after (C) contrast administration reveal consolidation in the right lower lobe with a rounded enhancing lesion inside the consolidated area (arrows).
With the recent worldwide resurgence of reported cases of Mycobacterium tuberculosis infection, recognition of complications and sequelae is important. Hemoptysis – often massive – in the presence of TB can have various etiologies, such as bronchiectasis, aspergilloma, TB reactivation, scar carcinoma, chronic bronchitis, microbial colonization within a cavity, and vascular complications such as pseudoaneurysms.3 Pulmonary artery pseudoaneurysms secondary to pulmonary TB are known as Rasmussen aneurysms and are caused by destruction of the media of segmental pulmonary arteries by granulation tissue from adjacent cavitary TB.1,4,5 Massive hemoptysis associated with chronic cavitary TB usually results from the rupture of a pseudoaneurysm through the cavity wall, and is potentially fatal.1,4,5
The diagnosis of Rasmussen aneurysm can be made readily on the basis of characteristic imaging findings. Chest radiographic findings that may suggest the formation of a pseudoaneurysm include intracavitary protrusion, the replacement of a cavity by a nodule, and a rapidly growing mass.4 Rasmussen aneurysm can be identified on pre- and post-contrast-enhanced CT images as avidly enhancing nodules located within the walls of tuberculous cavities2 or consolidations.
The optimal management of massive hemoptysis is currently under debate.5 Endovascular occlusion of the neck of the pulmonary aneurysm is well described in the literature and is usually successful in treating RA.1,5 Possible complications of treatment are bleeding recurrence, inadvertent embolization of a spinal artery leading to ischemic myelopathy, and aneurysmal rupture during diagnostic catheter angiography,1,5 with a high risk of mortality. Surgical excision is recommended only when expert radiological intervention is not available or in the presence of considerable destructive process in the lung.5
In conclusion, Rasmussen aneurysm should be included in the differential diagnosis of hemoptysis in patients with TB. Enhanced CT examination plays an important role in the evaluation of these patients.
Please cite this article as: Domingos-Grando R, Zanetti G, Marchiori E. Hemoptisis en tuberculosis: la importancia de la tomografía computarizada con contraste. Arch Bronconeumol. 2016;52:173–174.