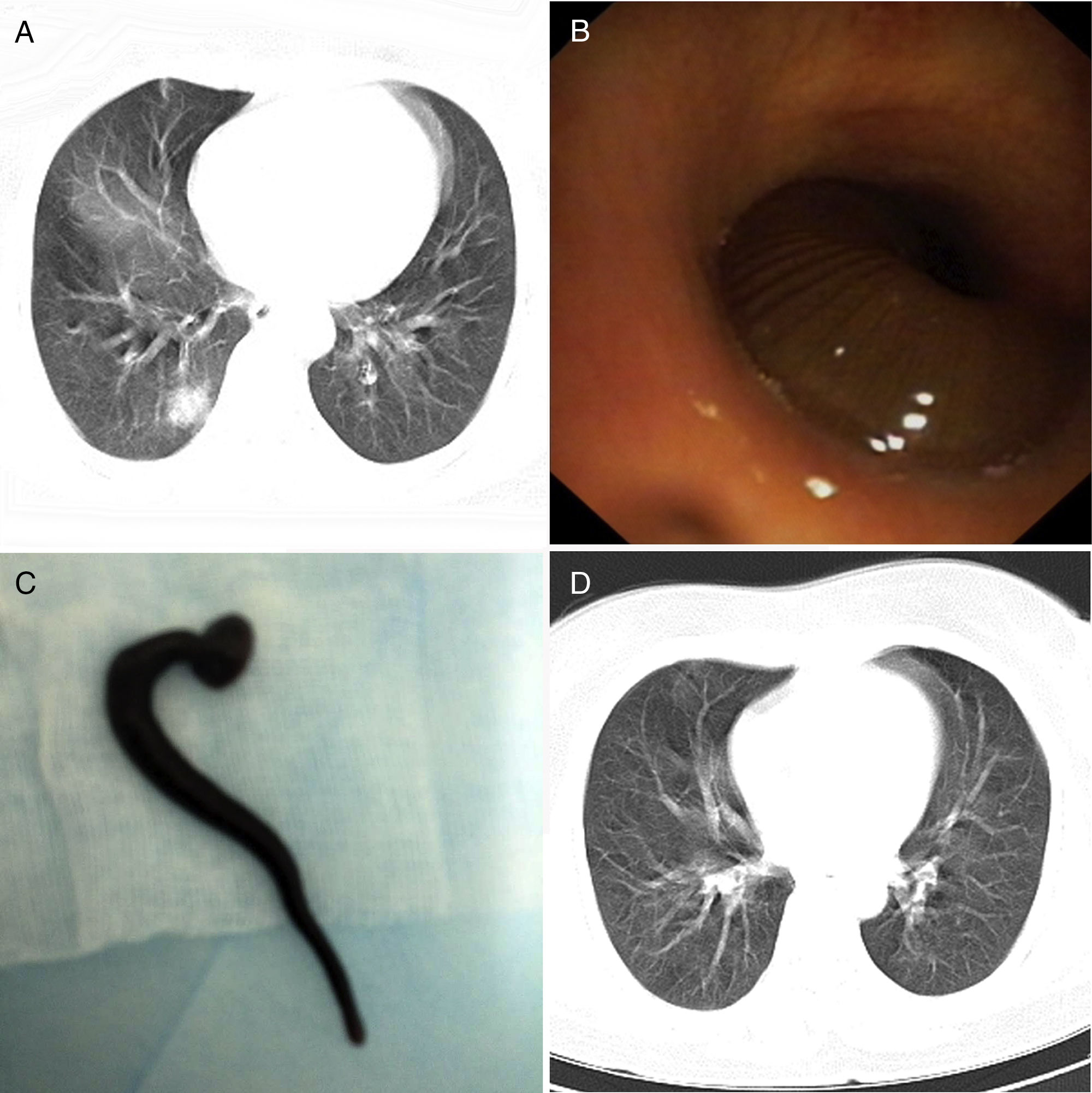
We report the case of a 49-year-old woman, who presented with a 6-week history of cough, rusty brown sputum with hemoptysis and hoarseness. She was a farmer and had a history of drinking field unboiled water. A computed tomographic scan of the chest showed a ground-glass opacity (GGO) in the medial basal segment of the right lower lobe, measuring 22mm in its largest diameter (Fig. 1A). Laboratory investigations demonstrated a white-cell count of 5280 per mm3 (reference range, 4000–10,000), an absolute eosinophil count of 600 per mm3 (reference range, 50–500), hemoglobin level of 147.00g/L (reference range, 110–160), and C-reactive protein levels of 11.30ml/L (reference range, 0 068–8.2). The blood coagulation tests were normal. The differential diagnosis included lung cancer, eosinophilic lung disease and focal pneumonia. Bronchoscopy was performed, and revealed a brown worm-like moving foreign body almost completely obstructing the lumen of the medial basal segmental bronchus of the right lower lobe (Fig. 1B). The foreign body was removed from the bronchus by cryoadhesion with a cryotherapy probe passed through the channel of a flexible bronchoscope with resolution of the obstruction and was identified as a 4cm long living leech (Fig. 1C). After removal of the leech, the patient was discharged from the hospital without any discomfort and complaint. Follow-up computed tomographic of the chest at 1 week showed the ground-glass opacity in the right lower lobe was almost completely resorbed (Fig. 1D).
Chest computed tomography showed a ground-glass opacity in the medial basal segment of the right lower lobe (A). Bronchoscopy revealed a brown worm-like moving foreign body almost completely obstructing the lumen of the medial basal segmental bronchus of the right lower lobe (B). The foreign body was identified as a 4cm long living leech (C). Chest computed tomography after 1 week showed the ground-glass opacity in the right lower lobe was almost completely absorbed (D).
Leeches are parasites that live in quiet pools and streams. Leeches are the very rare cause of airway foreign body around the world.1–3 Leeches are hemophagic parasites, living on occasional meals of blood obtained by attaching to fish, amphibians, and mammals. They can enter the human body when people drink infested water from quiet streams, pools and springs. Although there are several case reports about leech in the airway, these leeches locate in the larynx or trachea.1–3 Interestingly, the leech of our case was in the bronchus, and the chest CT showed a GGO. To the best of our knowledge, this is the first report of endobronchial leech showing a GGO on CT scan. The nature of this GGO induced by the parasite was unclear. We speculated that the cause might relate to blood tracking back into the parenchyma or an inflammatory response to the leech or its secretions. The differential diagnosis of GGO induced by endobronchial leech included lung cancer, eosinophilic lung disease and focal pneumonia.
Although extremely rarely seen, endobronchial leech infestation should be kept in mind especially in patients presenting with unexplained haemoptysis, hoarseness and elevated eosinophils and a history of drinking infested water from streams, pools and springs.
FundingThis work was supported by the “Special and Joint Program” of Yunnan Provincial Science and Technology Department and Kunming Medical University (No. 2014FA018), Science and Technology Program for Public Wellbeing of Yunnan Province (No. 2014RA020), and Young academic and technical leaders of Yunnan Province (No. 2017HB053).