Mediastinal masses are uncommon and include a large variety of entities. Half of them are located in the anterior mediastinum and up to 59% are malignant. Primary mediastinal lymphomas (PML) account for 10% of all mediastinal lymphomas and are defined as involvement of mediastinal lymph nodes, the thymus, and/or extranodal mediastinal organs without systemic disease. The most frequent PML are Hodgkin's lymphoma (HL) (50–70%) while non-Hodgkin's lymphoma (NHL) corresponds to 5–25% of them.1 We present a case series of a gray zone lymphoma (GZL) which is the missing link between NHL and HL.
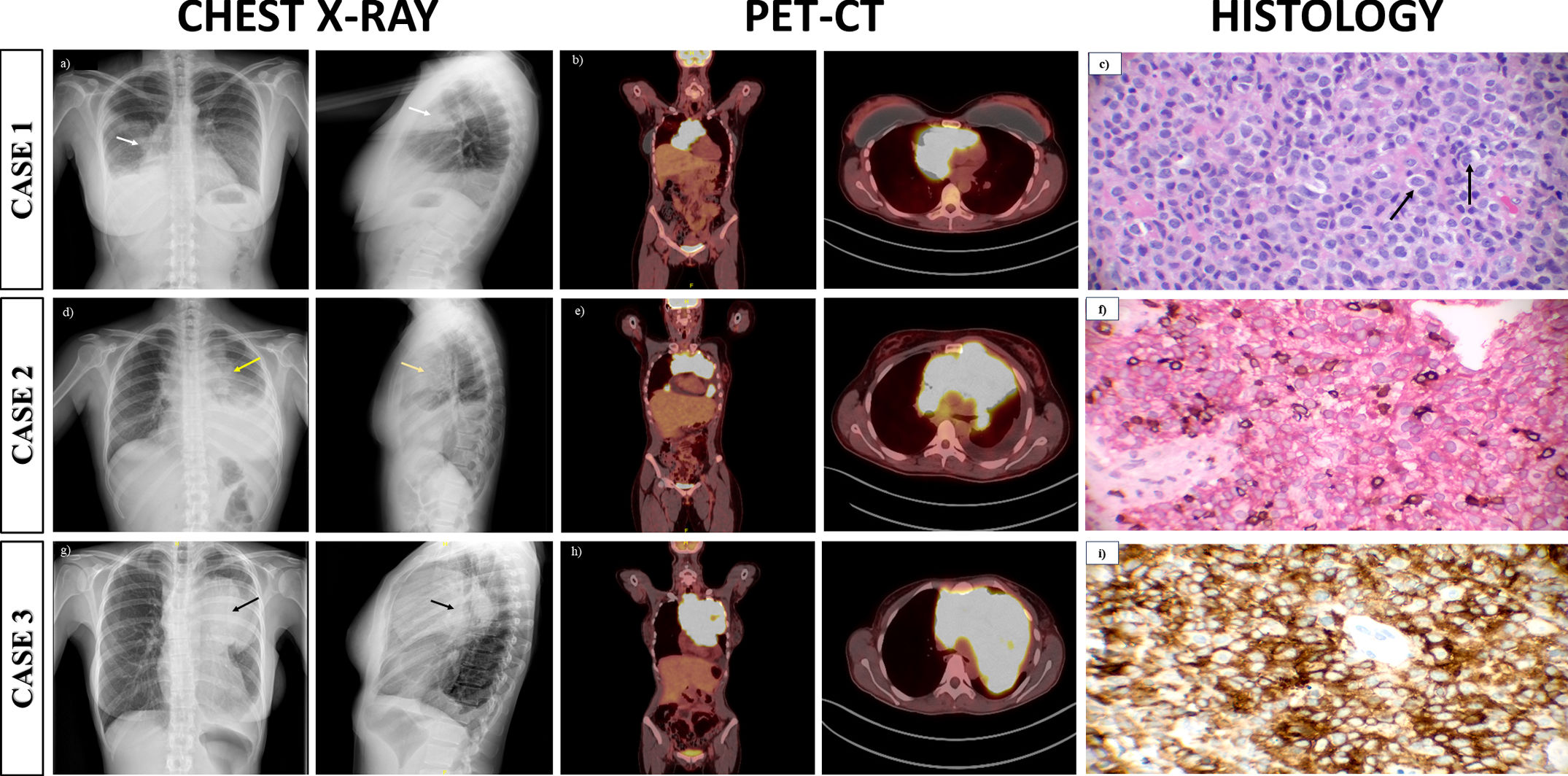
Over the course of a year, three women aged 39, 25 and 49 years were admitted for dyspnea and chest pain with chest X-rays compatible with anterior mediastinal masses (Fig. 1a, d, g). During admission, PET-CTs were carried out (Fig. 1b, e, h) showing anterior mediastinal masses with high maximum standardized uptake values (SUVmax). Diagnosis was made by bronchoscopy with biopsies that confirmed GZL with same phenotype: CD45+, CD20+, CD79a+, OCT 2+ PAX5+, CD10− BCL6 variable positivity, CD30+, CD15 variable positivity, MUM1/IRFA4+ and Epstein–Barr virus negative (Fig. 1c, f, i). Regarding complications, cases 2 and 3 presented cardiac tamponade and superior vena cava syndrome. All patients followed treatment with DA-EPOCH-R regimen (dose-adjusted etoposide, doxorubicin, cyclophosphamide, vincristine, prednisone and rituximab) presenting a complete response at 12 months.
(a) Posteroanterior and lateral chest radiograph a mass in the anterior mediastinum (white arrow) with middle lobe atelectasis and elevation of the right hemidiaphragm. (b) Positron emission tomography-computed tomography (PET-CT) with an anterior mediastinal mass (9cm×8cm×12cm) with higher maximum standardized uptake values (SUVmax) of 24, with invasion of the phrenic nerve. (c) Large cells with centroblastic appearance and pleomorphism in an inflammatory background and fibrotic stroma with resembling Reed-Sternberg cells (black arrow) (hematoxylin–eosin, original magnification 400×). (d) Posteroanterior and lateral chest radiograph with an anterior mediastinal mass (yellow arrow) and left pleural effusion. (e) PET-CT with a 14cm×13cm×15cm mass in the anterior mediastinum with a SUVmax of 19 with compression of the superior vena cava and adenopathies. (f) Immunohistochemical stainin with neoplastic cells with expression of CD20 (original magnification 400×). (g) Posteroanterior and lateral chest radiograph with anterior mediastinal mass (black arrow) with left pleural effusion. (f) PET-TC with a 13cm×14cm×17cm mass in the anterior mediastinum with a SUVmax of 19.6 and compression of the superior vena cava. (i) Malignant cells with strongly expression of CD30 (original magnification 400×).
Lymphomas are neoplasms that result from excessive clonal proliferation of B lymphocytes, T lymphocytes or the natural killer cells during maduration. NHL constitutes about 80–90% of all lymphomas being the most common hematological neoplasm with a variety of histologic presentations. Gray zone lymphoma (GZL) is a B-cell lymphoma which can be classified as HL or NHL. Currently is defined as a B-cell lymphoma with features between sclerosis nodular lymphoma (SNL) and Primary Mediastinal B-cell Lymphoma (PMBL).2 The estimated incidence rate is 0.52 per million person-years with an overall survival of 80% at 34 months of follow-up. It affects young patients and children with a predominance in men of 1.4:1, unlike LH and PMBL. It manifests in up to half of the patients as an anterior mediastinal mass that may be associated with superior vena cava syndrome or cardiac tamponade. Extranodal involvement is exceptional. Histologically, tumor cells present centroblastic or immunoblastic appearance and pleomorphism. Reed-Sternberg cells may be visualized but of smaller size and with less prominent nuclei. Immunophenotype of GZL is variable with transitional and divergent patterns. The characteristic immunophenotype of GZL is: CD20+, CD30+, CD79a+, PAX5+, OCT2+ and MUM1/IRF4+. The positivity of bcl6, CD15 and CD45 were variable whereas the positivity of CD10 and Epstein–Barr virus are uncommon.3
The most administered and effective treatment is DA-EPOCH-R which is the same treatment of primary B-cell lymphoma (PMBL). The event-free survival (EFS) rate at a median follow-up of 59 months was 62% and the overall survival (OS) rate was 74% at a median follow-up of 59 months. However, the response to treatment was worse than that observed in PMBL at a median follow-up of 5 years (EFS: 93% and OS: 97%).4
Other available treatments are CHOP±R (cyclophosphamide, doxorubicin, vincristine and prednisone±rituximab) and ABVD±R (doxorubicin, bleomycin, vinblastine and dacarbazine±rituximab) with an overall response rate (ORR) of 65% and 60%, respectively.3 Other treatments that are effective include escBEACOPP (methylprednisolone, doxorubicin, cyclophosphamide, procarbazine, etoposide, bleomycin and vincristine) and ACBVP (doxorubicin, methylprednisolone, cyclophosphamide, bleomycin and vindesine) with longer 3-years OS (94% and 86%, respectively) than R-CHOP (OS=75%) and ABVD (OS=61%)7. In terms of new biologic therapies, anti-CD30 antibody drug conjugates such as brentuximab vedotin are an option for CD30-expressing GZL. Programmed cell death protein 1 (PD-1) is being investigated as a potential therapeutic target.5
In conclusion, GZL is a lymphoma intermediate between HL and PMBL with an aggressive clinical course. Its diagnosis is a challenge for the pathologist due to its histological similarity to both HL and NHL. There is a lack of treatment guidelines, so it is important to conduct large multicentre studies to develop consensus guidelines.
FundingThis work has not received funding of any kind.
Conflict of interestThe authors declare that they have no conflict of interest directly or indirectly related to the contents of the manuscript.