Pulmonary rehabilitation (PR) including exercise training is a recognized cornerstone of comprehensive management of chronic obstructive pulmonary disease (COPD).1,2 Despite well documented effects only about 10% of potential candidates are currently referred to PR, access to programs is challenged by lack of facilities, transportation, costs, and geographical obstacles.1–3
To increase access to programs, governments should develop policies to increase resources, logistics, availability and expertise of healthcare providers, including telerehabilitation programs.3,4 However there is also the need to define priority criteria, not to “waste” available resources for candidates with few probabilities of success. The role of gender and age in success of PR is still discussed. Evidence suggests sex-related differences in compliance with rehabilitation programs of individuals with COPD.5 In addition, studies with limited sample sizes highlight age and sex differences in balance outcomes among individuals with COPD at risk of falls.6 Therefore, this large retrospective multicentric study assesses whether demographic characteristics might influence response to PR in exercise capacity.
The study was approved by the Ethics Committee (2164 CE, 5 December 2017 and 2555 CE 8 June 2021). Participants did not provide any specific informed consent, however, at admission they had given informed consent for the scientific use of their clinical data. As a retrospective analysis, the study was not registered. Part of the data has been published elsewhere.7–9
This study was conducted on data of individuals with diagnosis of COPD consecutively admitted between January 2010 and October 2017 to Montescano hospital and from January 2018 to December 2021 to other hospitals of ICS Maugeri network (Lumezzane, Pavia, Tradate, Veruno, Milano, Telese Italy). These hospitals share the same evaluation tools and rehabilitation programs.
Only data of individuals with baseline lung function and paired prior and post-program data of exercise tolerance were analyzed. Inclusion criteria to the study were: age >40 years; diagnosis of COPD (post-bronchodilator forced expiratory volume at 1s (FEV1)<80% predicted, and FEV1/forced vital capacity (FVC)<70%)2; admission within 30 days after an exacerbation; stable conditions. Exclusion criteria were: oncological, neurological, heart failure, ischemic cardiovascular diseases; inability or denial to perform evaluations or PR.
Demographics, anthropometrics, length of hospital stay (LoS), prevalence of Global strategy for prevention, diagnosis and management of COPD (GOLD) airflow stages,2 comorbidities by the Cumulative Illness Rating Scale (CIRS) were recorded. At admission, dynamic lung volumes were assessed according to standards.
Before and after the program, exercise tolerance was assessed by the 6-min walking-test (6MWT). Data are shown as meters and percent of predicted values. The minimal clinically important difference (MCID) in individuals with COPD has been reported as an improvement by at least 30m.10
Our multidisciplinary program consists of 6 weekly, 2–3h sessions including 30min supervised cycle endurance training, setting the initial load at 50–70% of the maximal load calculated according to the baseline 6MWT, increasing or decreasing the load according to dyspnea level as previously described.7 It included also abdominal, upper and lower limb muscle strength exercises and optimization of drug therapy, education, nutritional and psychosocial counseling when needed. Participants were considered as completers when attending at least 12 sessions.11
Descriptive statistics are reported as mean±SD for continuous and as numbers (N) and percentage (%) for discrete variables. Between-group comparisons for continuous variables were carried out by unpaired t-test (two groups) or one-way analysis of variance (ANOVA, three groups) with post hoc analysis if appropriate and Chi-square test for categorical variables. The association between couples of variables was assessed by Pearson's correlation coefficient. The association between the post-program changes in 6MWT (Δ6MWT) and variables was assessed by linear regression model analysis. All statistical tests were two-tailed and statistical significance was set at p<0.05.
Out of 2137 individuals with COPD (FEV1/FVC<70%) admitted in the study period, 681 were excluded due to missing 6MWT data, 5 died, 77 were transferred to acute care hospitals, and 23 were not completers. Data from 1351 individuals (67.7% males) were analyzed. Males were slightly but significantly older, had more comorbidities, and a shorter LoS. Airflow obstruction was slightly but significantly more severe in males whereas females showed significantly lower levels of serum hemoglobin. As expected, there were differences in baseline and post-program walked meters but not in 6MWT, %predicted, or in Δ6MWT (Table 1, Panel A).
Demographic, anthropometric, physiological, and clinical characteristics.
| Variable | All patients (N=1351) | Males (N=915) | Females (N=436) | p-Value |
|---|---|---|---|---|
| Panel A. According to sex | ||||
| Age, years | 70.4±8.7 | 70.7±8.7 | 69.6±8.7 | 0.03 |
| BMI, kg/m2 | 26.9±6.3 | 27.2±5.9 | 26.5±7.1 | 0.05 |
| CIRS, score | 3.69±1.92 | 3.81±2.00 | 3.44±1.70 | 0.01 |
| LoS, days | 27.7±11.3 | 27.2±11.2 | 28.7±11.7 | 0.02 |
| FEV1, % pred | 47.8±19.1 | 47.7±19.0 | 48.1±19.5 | 0.70 |
| FVC, % pred | 74.2±19.7 | 73.7±19.0 | 75.2±21.0 | 0.19 |
| FEV1/FVC, % pred | 48.3±11.2 | 47.9±11.4 | 49.2±10.8 | 0.04 |
| GOLD I, n (%) | 94 (7.0) | 61 (6.6) | 33 (7.6) | 0.54* |
| GOLD II, n (%) | 392 (29.0) | 268 (29.3) | 124 (28.4) | 0.75* |
| GOLD III, n (%) | 665 (49.2) | 450 (49.2) | 215 (49.3) | 0.96* |
| GOLD IV, n (%) | 200 (14.8) | 136 (14.9) | 64 (14.7) | 0.93* |
| Serum Hb, g/L | 13.1±1.8 | 13.4±1.8 | 12.5±1.6 | <0.0001 |
| Admission 6MWT, m | 305.3±122.9 | 314.8±123.1 | 285.3±120.1 | <0.0001 |
| Discharge 6MWT, m | 354.2±115.7 | 362.6±116.6 | 336.4±111.9 | <0.0001 |
| Δ6MWT, m | 48.9±66.2 | 47.9±67.5 | 51.1±63.6 | 0.40 |
| Admission 6MWT, % pred | 66.2±26.6 | 67.0±26.8 | 64.6±26.2 | 0.14 |
| Discharge 6MWT, % pred | 76.9±25.4 | 77.1±25.6 | 76.4±24.9 | 0.64 |
| Δ6MWT, % pred | 10.7±14.5 | 10.2±14.3 | 11.8±14.8 | 0.06 |
| Variable | ≤67 years (N=468) | >67≤74 years (N=430) | >74 years (N=453) | p-Value# |
|---|---|---|---|---|
| Panel B. According to age | ||||
| Age, years | 60.9±5.7 | 71.2±1.9 | 79.4±3.6 | <0.0001 |
| BMI, kg/m2 | 27.1±7.2 | 26.6±6.0 | 27.1±5.5 | 0.42 |
| CIRS, score | 3.21±1.71 | 3.88±1.86 | 4.10±2.10 | <0.0001 |
| LoS, days | 26.9±10.6 | 28.0±12.4 | 28.1±10.9 | 0.21 |
| FEV1, % pred | 45.3±17.7 | 47.7±19.4 | 50.6±20.0 | 0.00013 |
| FVC, % pred | 73.0±18.8 | 74.3±20.8 | 75.3±19.4 | 0.21 |
| FEV1/FVC, % pred | 47.4±12.1 | 47.8±10.8 | 49.8±10.4 | 0.004 |
| Serum Hb, g/L, | 13.43±1.82 | 13.23±1.80 | 12.70±1.70 | <0.0001 |
| Admission 6MWT, m | 336.9±119.9 | 306.4±125.7 | 271.5±114.4 | <0.0001 |
| Discharge 6MWT, m | 390.9±109.9 | 353.6±115.9 | 316.8±109.4 | <0.0001 |
| Δ6MWT, m | 54.0±71.9 | 47.2±64.1 | 45.2±61.8 | 0.11 |
| Admission 6MWT, % pred | 65.4±24.1 | 66.3±27.4 | 67.0±28.4 | 0.67 |
| Discharge 6MWT, % pred | 75.8±22.7 | 76.8±26.0 | 78.1±27.3 | 0.39 |
| Δ6MWT, % pred | 10.44±14.25 | 10.44±14.23 | 11.17±15.05 | 0.69 |
BMI: body mass index; CIRS: Cumulative Illness Rating Scale; LoS: length of stay; FEV1: forced expiratory volume in the 1st second; % pred: percentage of predicted; FVC: forced vital capacity; GOLD: global strategy for prevention, diagnosis and management of COPD stage; Hb: hemoglobin; 6MWT: six-minute walking test.
Participants were also grouped according to age tertiles: ≤67, >67 and ≤74, and >74 years. As expected airway obstruction, exercise capacity, and occurrence of comorbidities significantly worsened with age. However, there was no age-related significant difference in baseline 6MWT, % predicted or in Δ6MWT (Table 1, Panel B).
After the program 63.4% of participants reached the MCID for 6MWT without any significant difference in gender (males: 63.6%, females: 63.8%, p=0.96), age (64.1%, 62.1%, 64.7% for increasing age tertiles respectively, p=0.70) or GOLD stages (67.0%, 61.2%, 64.1%, 65.5%, p=0.61).
As compared to older, young males improved their 6MWT in meters but not in % predicted (Δ6MWT: 57.2±73.7 vs. 45.2±61.9 and 41.4±65.4m for increasing age tertiles respectively, p=0.010). Females did not show any significant age-related difference in Δ6MWT. However, females over 67 years showed a significantly higher Δ6MWT than their male peers both in meters (52.9±60.6 vs. 43.3±63.7m respectively, p=0.03) and in % predicted (12.8±14.6 vs. 9.9±14.6%, respectively, p=0.007). The only slight significant baseline difference was in airflow obstruction (FEV1/FVC: 48.3±10.9 vs. 49.9±10.1%, in males and females over 67 respectively, p=0.046).
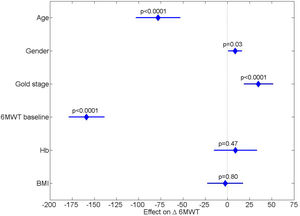
In both genders, there was a highly significant inverse correlation between Δ6MWT and baseline 6MWT (Pearson's r −0.37, p<0.0001 for meters and −0.38, p<0.0001 for % predicted). A weaker correlation was observed only for Hb (r: −0.10, p=0.0008). Among considered variables, only age, gender, GOLD stage and baseline 6MWT were significantly and independently associated with Δ6MWT (Fig. 1).
Graphical representation of the effect of the considered predictors on post program change in 6MWT (Δ6MWT). Diamonds represent the expected average change in Δ6MWT moving from one extreme value to the other of each variable, adjusted for all other variables. The lines around the diamonds represent the 95% confidence interval: crossing the zero effect line indicates lack of significance. Abbreviations: BMI: body-mass index; 6MWT: 6-minute walking-test; GOLD: global strategy for prevention, diagnosis and management of COPD.
Finally, data of 436 participants included from March 2020 to December 2021 (Covid-19 pandemic) did not show any significant difference in anthropometrics, comorbidities occurrence or response to program as compared to prior 2020. The only negligible albeit significant differences were in age (71.2±8.8 vs. 69.9±8.6 years, in 2020–2021 and prior 2020 respectively, p=0.011) and airflow obstruction (FEV1/FVC: 47.4±9.9 vs. 48.8±11.7%, p=0.039).
This large retrospective, multicentric study shows that in individuals with COPD gender or age do not influence success of PR in improving exercise capacity, however older females get a greater benefit than their male peers.
Despite well-documented positive effects,1,2 there are limitations to access to programs as required by clinical indications.3 In addition to policies to increase access, we should consider also priority criteria to limit or postpone access to individuals with low probability of success (non responders).
We have used the ability to reach the MCID in 6MWT as a marker of responder to PR. Different criteria have been used to define responders including differences in outcome measures (such as exercise capacity, symptoms, or quality of life) and/or in size of improvement such as % of baseline values. More recently a multidimensional evaluation has been suggested.12
The role of gender difference in outcome of COPD as well in success of PR is still discussed.5,6,13,14 A systematic review showed that there is insufficient evidence to support gender-associated differences in PR outcomes.14
As compared to previous ones, our study confirms the benefits of PR adding the proportion of responders (reaching the MCID) and results of 6MWT as % of predicted values. The use of predicted values avoids bias related to gender or age differences in exercise capacity (Table 1).
While confirming that overall age does not influence success rate of PR,15 our study adds the interesting information on interaction between age and sex showing that older females get a greater benefit than their male peers. The only (albeit slight) significant difference in available data between males and females over 67 was in airflow obstruction. Other factors, such as compliance to program cannot be excluded on the basis of our data.
In agreement with other studies12 our study confirms that individuals with most severe limitation in exercise capacity are those with higher probability of success of PR. Our study shows also that BMI or serum Hb do not influence success rate (Fig. 1).
Data entry was conducted also during Covid-19 pandemic (2020–2021). While influencing services (need to offer care for post-acute and long-Covid), results of our study were not substantially affected.16
This is a retrospective study with flaws of these studies such as missing data. A high proportion of exclusions (31.9% of eligible participants) was due to missing 6MWT data. Data of drug therapy of most of analyzed individuals were missing, therefore we cannot exclude any potential drug effect on results. The lack of a control population not performing PR might be criticized. However, given the well-recognized benefits (as also this study confirms), not performing exercise training would have been unaethical. The reported comorbidities occurrence in our study must not be considered as a real prevalence as our participants did not undergo any specific diagnostic test.
In conclusion, in individuals with COPD, gender or age do not influence success rate in exercise capacity of PR, however, older females get a greater benefit than their male peers. These results may be useful to define admission criteria to programs.
Authorship contributionsMV, MP and NA conceived and designed the study. MV and NA contributed to the writing of the manuscript. RM performed formal analysis. RM, MV, MP, EZ and NA participated in the analysis and discussion of the data, revised the article critically and approved the final version.
FundingThis work was supported by the “Ricerca Corrente” Funding scheme of theMinistry of Health, Italy.
Conflict of interestsThe authors declare they have no conflict of interest.
The Authors thank Adriana Olivares for her technical assistance and editing.