A middle-aged woman with presumed mesothelioma presented with dyspnea and recurrent right pleural effusion. At the time of her initial diagnosis at an outside institution, she had a right pleural effusion and right pleural based thickening. Cytology from thoracentesis revealed only atypical cells, and histologic diagnosis from a CT-guided biopsy of right pleura concluded possible mesothelioma versus primary lung carcinoma. She was treated with erlotinib followed by sorafenib. She presented to our institution 6 months later for a second opinion. Staging and video-assisted thoracoscopic surgery with talc pleurodesis of the right hemithorax was then performed to ascertain pathologic diagnosis. Multiple pleural based nodules with mucinous material covering both the visceral and parietal pleural were visualized, and thick mucinous material was suctioned from the right chest. Pathology confirmed epithelioid malignant mesothelioma. She declined further systemic therapy at the time, but she returned 5 months later with worsening shortness of breath. Chest radiograph showed opacification of the right hemithorax with deviation of the trachea contralaterally. Thoracentesis on the right hemithorax yielded 2.1L of thick jelly-like fluid. Due to reaccumulation of the fluid, an indwelling pleural catheter (IPC) was placed 2 weeks later. Patient was started on chemotherapy with carboplatin and pemetrexed for 6 cycles and then continued maintenance pemetrexed. The IPC was drained daily and removed 18 months after placement. She did not have any catheter-related infection or malfunction. She later returned abroad for alternative therapies. The patient expired due to progressive disease.
Gelatinous pleural effusion may present a diagnostic and therapeutic challenge. Hyaluronic acid produced by malignant mesothelioma is thought to contribute to its viscous appearance, and elevated levels in the pleural fluid supports the diagnosis of mesothelioma compared to other cancers.1 The thixotropic pleural fluid exhibits a change in viscosity depending on the degree and duration of force applied, and in the case of pleural effusion, it allows for drainage of the fluid with prompt return to a jelly-like consistency when stagnant. Other potential etiologies of viscous pleural effusion may include other cancers and infection (tuberculosis, paragonimiasis).2 Malignancy-related gelatinous pleural fluid have also been associated with melanoma, lung cancer, myxoid sarcoma of the pleura, multiple myeloma, and abdominal or gynecologic (including pseudomyxoma peritonei) tumors.3 IPCs have become the mainstay for the care and palliation of malignant pleural effusions (MPE), and since MPE reoccurred despite talc pleurodesis, IPC provided symptom palliation and helped avoid additional procedures (Fig. 1).
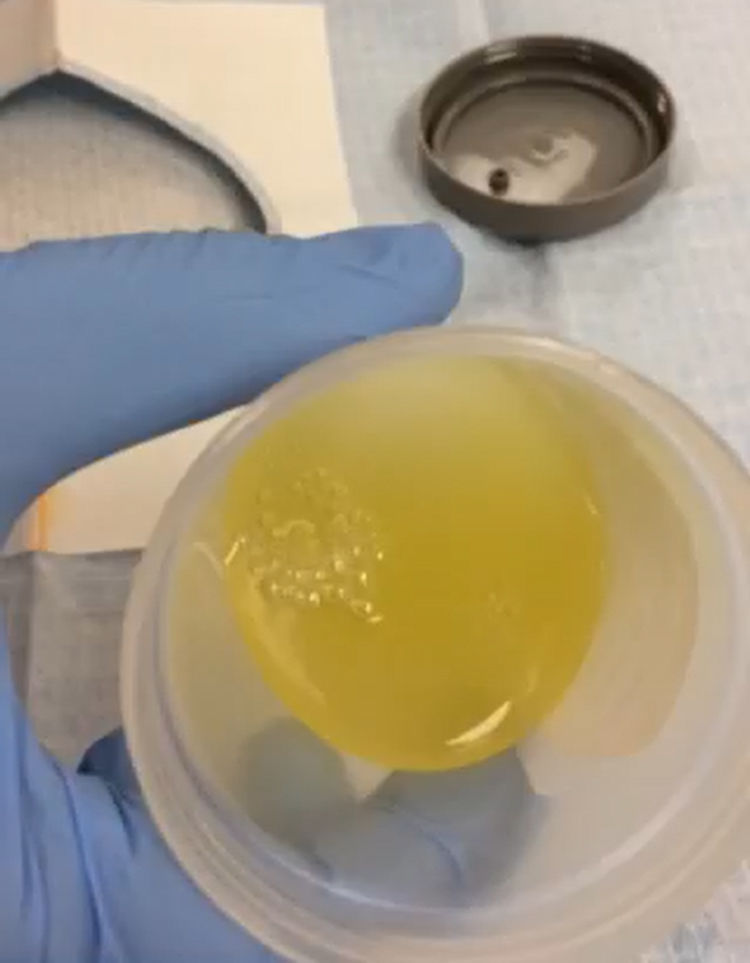
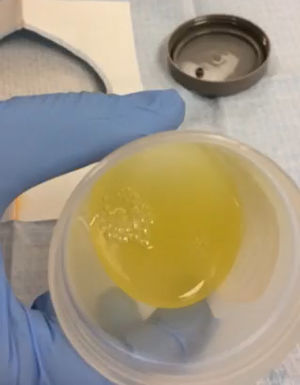
Supplementary video file. Pleural effusion is thick and yellow as it is poured into the specimen cup. The fluid has thixotropic properties where it stable at rest but appears to become more fluid when agitated. Limited pleural fluid analysis revealed an elevated total protein of 3.1, cell count of 950 WBCS with 1 neutrophil, 98 mononculear and 1 other. Cultures were negative. Cytology reveals rare atypical cells in a background of abundant mucoid material.
This research is supported in part by the National Institutes of Health through MD Anderson's Cancer Center Support Grant (CA016672).