Frequent attendance (FA) is an excessive use of health services according to a patient's risk profile. In the primary care setting, patients with chronic obstructive pulmonary disease (COPD) are the most frequent attenders, accumulating 10 or more medical visits annually.1 This greater demand has been associated with different determinants, such as a high number of comorbidities, functional status, quality of life, socioeconomic, demographic or organizational factors.2,3
FA affects patients, professionals and the healthcare system itself. Because of this, there is of great importance to ascertain the variables associated with this phenomenon. In the case of COPD patients, there is no composite picture of the effect of all the variables analyzed, which would serve to focus the analysis from the personal, clinical, healthcare and organizational perspectives that might affect the likelihood of becoming a frequently attending patient in the out-of-hospital setting.
The aim of this study was to ascertain the profile of COPD patients who are frequent attenders in the out-of-hospital setting by conducting a population-based case–control study. The study population consisted of national health cardholders from the Santiago de Compostela health area (Galicia, Spain) with a diagnosis of COPD prior to 2011, who were allocated to Primary Care Practitioners (PCPs) and had an active clinical episode of COPD as of 21/12/2016 in their electronic medical record (EMR) (ICPC-2 R95). Participants were required to have had a minimum of one spirometry test in the preceding three years, be over 35 years old, and have an active prescription of medications associated with obstructive diseases (R03 therapeutic group ATC). All patients had to be alive in December 2016 to be included.
We formed two groups of cases and one group of controls, classified according to the intensity of care requested from out-of-hospital settings (including PCPs and out-of-hospital emergency services) from December 2016 through December 2017. To establish these groups, the 75th percentile (P75) and the 90th percentile (P90) of care intensity during the period were defined as cutpoints. The following groups were formed: a control group of “non-frequent attenders” (NF) with 0–10 visits (
This study was approved by the Santiago-Lugo Research Ethics Committee under registry code 2016/196. All data were collected retrospectively and were obtained without any type of intervention or possible modification of the clinical disease course. Informed consent was not required.
The data were obtained via EMR and different health information systems. The following variables were collected: (a) socio-demographic characteristics; (b) smoking habit; (c) comorbidities: anxiety, depression and dementia; CHA2DS2-VASc score4: estimation of the risk of stroke in patients with atrial fibrillation, which predisposes to thrombo-embolic stroke; Clinical Risk Groups (CRG)5: the CRG assigned to each patient was obtained in accordance with the clinical information available from their EMR in order to predict future resource use; (d) spirometry test, date and place of performance; (e) visits to out-of-hospital settings; (h) pharmacological treatment; (i) home oxygen therapy. The presence of out-of-hospital settings in patients’ municipality of residence, distance to the hospital and number of deaths were recorded.
Multinomial logistic regression models were fitted to identify predictors of out-of-hospital attendance, using the NF group as reference. Odds ratios (ORs) and their 95% confidence intervals (95% CI) were calculated. The model's discrimination was analyzed using the area under the ROC curve (AUC), and its calibration using the Hosmer–Lemeshow test. All statistical analyses were performed using IBM SPSS Statistics v.19.0.
A total of 8861 persons had COPD in their EMR and of those 4274 were included in the study. No significant differences were observed by sex, however age was higher in the excluded group (71 vs 78). During the study period, 228 deaths occurred.
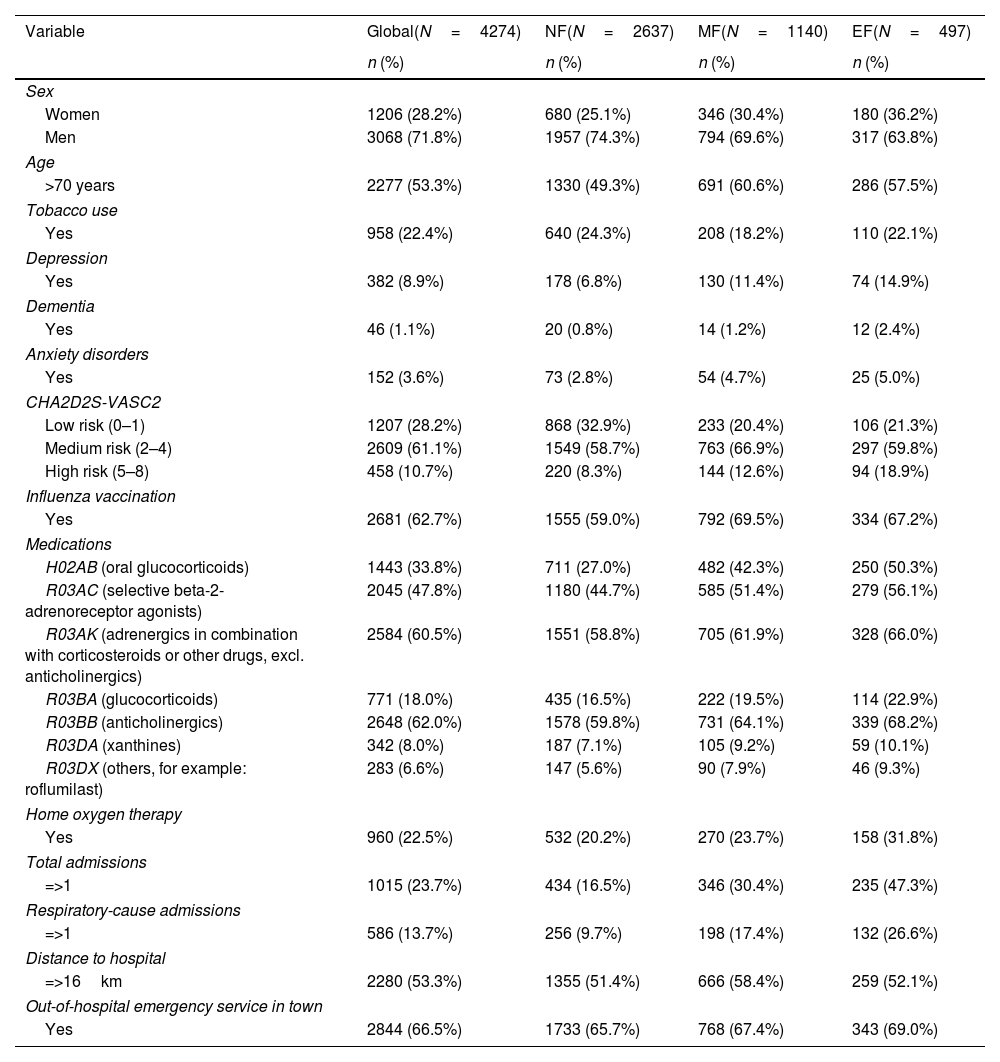
Of the 4274 subjects, 2637 (61.7%) were allocated to the NF, 1140 (26.7%) to the MF, and 497 (11.6%) to the EF attendance group. Table 1 shows the main characteristics of the participants.
Main characteristics of the study population.
| Variable | Global(N=4274) | NF(N=2637) | MF(N=1140) | EF(N=497) |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Sex | ||||
| Women | 1206 (28.2%) | 680 (25.1%) | 346 (30.4%) | 180 (36.2%) |
| Men | 3068 (71.8%) | 1957 (74.3%) | 794 (69.6%) | 317 (63.8%) |
| Age | ||||
| >70 years | 2277 (53.3%) | 1330 (49.3%) | 691 (60.6%) | 286 (57.5%) |
| Tobacco use | ||||
| Yes | 958 (22.4%) | 640 (24.3%) | 208 (18.2%) | 110 (22.1%) |
| Depression | ||||
| Yes | 382 (8.9%) | 178 (6.8%) | 130 (11.4%) | 74 (14.9%) |
| Dementia | ||||
| Yes | 46 (1.1%) | 20 (0.8%) | 14 (1.2%) | 12 (2.4%) |
| Anxiety disorders | ||||
| Yes | 152 (3.6%) | 73 (2.8%) | 54 (4.7%) | 25 (5.0%) |
| CHA2D2S-VASC2 | ||||
| Low risk (0–1) | 1207 (28.2%) | 868 (32.9%) | 233 (20.4%) | 106 (21.3%) |
| Medium risk (2–4) | 2609 (61.1%) | 1549 (58.7%) | 763 (66.9%) | 297 (59.8%) |
| High risk (5–8) | 458 (10.7%) | 220 (8.3%) | 144 (12.6%) | 94 (18.9%) |
| Influenza vaccination | ||||
| Yes | 2681 (62.7%) | 1555 (59.0%) | 792 (69.5%) | 334 (67.2%) |
| Medications | ||||
| H02AB (oral glucocorticoids) | 1443 (33.8%) | 711 (27.0%) | 482 (42.3%) | 250 (50.3%) |
| R03AC (selective beta-2-adrenoreceptor agonists) | 2045 (47.8%) | 1180 (44.7%) | 585 (51.4%) | 279 (56.1%) |
| R03AK (adrenergics in combination with corticosteroids or other drugs, excl. anticholinergics) | 2584 (60.5%) | 1551 (58.8%) | 705 (61.9%) | 328 (66.0%) |
| R03BA (glucocorticoids) | 771 (18.0%) | 435 (16.5%) | 222 (19.5%) | 114 (22.9%) |
| R03BB (anticholinergics) | 2648 (62.0%) | 1578 (59.8%) | 731 (64.1%) | 339 (68.2%) |
| R03DA (xanthines) | 342 (8.0%) | 187 (7.1%) | 105 (9.2%) | 59 (10.1%) |
| R03DX (others, for example: roflumilast) | 283 (6.6%) | 147 (5.6%) | 90 (7.9%) | 46 (9.3%) |
| Home oxygen therapy | ||||
| Yes | 960 (22.5%) | 532 (20.2%) | 270 (23.7%) | 158 (31.8%) |
| Total admissions | ||||
| =>1 | 1015 (23.7%) | 434 (16.5%) | 346 (30.4%) | 235 (47.3%) |
| Respiratory-cause admissions | ||||
| =>1 | 586 (13.7%) | 256 (9.7%) | 198 (17.4%) | 132 (26.6%) |
| Distance to hospital | ||||
| =>16km | 2280 (53.3%) | 1355 (51.4%) | 666 (58.4%) | 259 (52.1%) |
| Out-of-hospital emergency service in town | ||||
| Yes | 2844 (66.5%) | 1733 (65.7%) | 768 (67.4%) | 343 (69.0%) |
NF: non-frequent attenders; MF: moderately frequent attenders; EF: extremely frequent attenders.
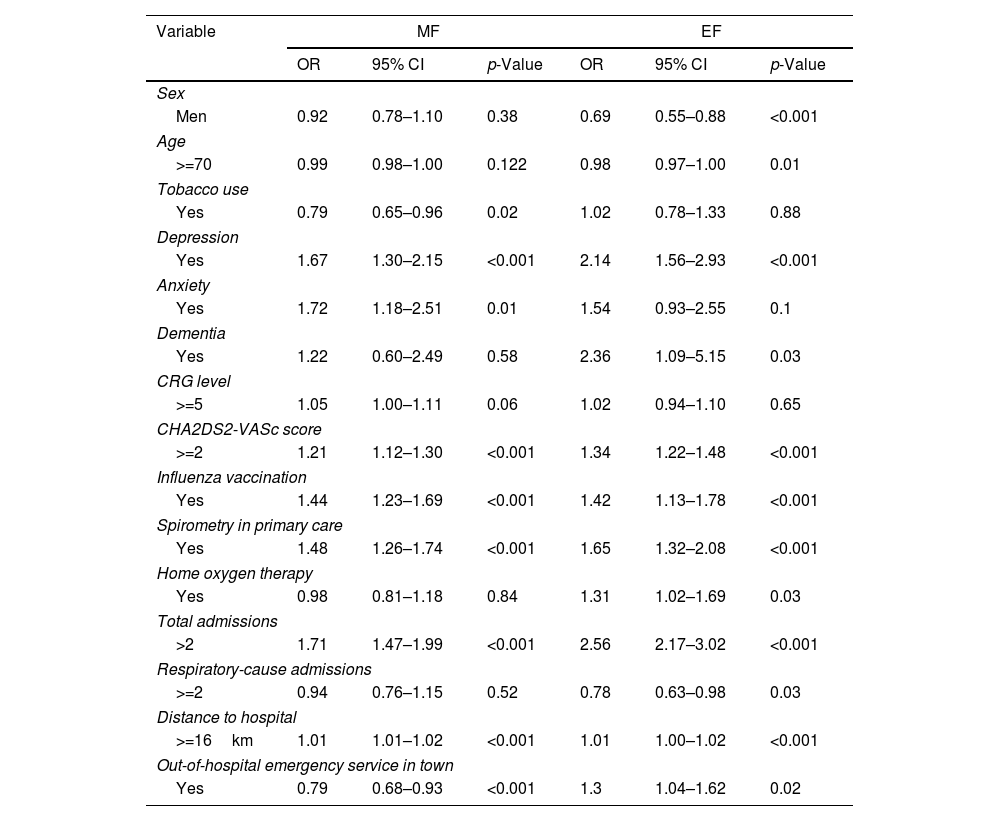
Presence of anxiety, depression and number of re-admissions were the factors most closely associated with MF attendance. In contrast, the profile of EF attenders was mainly determined by presence of dementia, depression and number of re-admissions (Table 2).
Multinomial logistic regression, adjusted for age and sex.
| Variable | MF | EF | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Sex | ||||||
| Men | 0.92 | 0.78–1.10 | 0.38 | 0.69 | 0.55–0.88 | <0.001 |
| Age | ||||||
| >=70 | 0.99 | 0.98–1.00 | 0.122 | 0.98 | 0.97–1.00 | 0.01 |
| Tobacco use | ||||||
| Yes | 0.79 | 0.65–0.96 | 0.02 | 1.02 | 0.78–1.33 | 0.88 |
| Depression | ||||||
| Yes | 1.67 | 1.30–2.15 | <0.001 | 2.14 | 1.56–2.93 | <0.001 |
| Anxiety | ||||||
| Yes | 1.72 | 1.18–2.51 | 0.01 | 1.54 | 0.93–2.55 | 0.1 |
| Dementia | ||||||
| Yes | 1.22 | 0.60–2.49 | 0.58 | 2.36 | 1.09–5.15 | 0.03 |
| CRG level | ||||||
| >=5 | 1.05 | 1.00–1.11 | 0.06 | 1.02 | 0.94–1.10 | 0.65 |
| CHA2DS2-VASc score | ||||||
| >=2 | 1.21 | 1.12–1.30 | <0.001 | 1.34 | 1.22–1.48 | <0.001 |
| Influenza vaccination | ||||||
| Yes | 1.44 | 1.23–1.69 | <0.001 | 1.42 | 1.13–1.78 | <0.001 |
| Spirometry in primary care | ||||||
| Yes | 1.48 | 1.26–1.74 | <0.001 | 1.65 | 1.32–2.08 | <0.001 |
| Home oxygen therapy | ||||||
| Yes | 0.98 | 0.81–1.18 | 0.84 | 1.31 | 1.02–1.69 | 0.03 |
| Total admissions | ||||||
| >2 | 1.71 | 1.47–1.99 | <0.001 | 2.56 | 2.17–3.02 | <0.001 |
| Respiratory-cause admissions | ||||||
| >=2 | 0.94 | 0.76–1.15 | 0.52 | 0.78 | 0.63–0.98 | 0.03 |
| Distance to hospital | ||||||
| >=16km | 1.01 | 1.01–1.02 | <0.001 | 1.01 | 1.00–1.02 | <0.001 |
| Out-of-hospital emergency service in town | ||||||
| Yes | 0.79 | 0.68–0.93 | <0.001 | 1.3 | 1.04–1.62 | 0.02 |
MF: moderately frequent attenders; EF: extremely frequent attenders; OR: odds ratio; 95% CI: 95% confidence interval; CRG: clinical risk group.
The fitted models showed acceptable discrimination in the case of EF attendance (AUC: 0.72 [95% CI 0.69–0.74; p<0.0001]) but this was not so for the model of MF attendance (AUC: 0.61 [95% CI 0.59–0.63; p<0.0001)].
According to our results, age, sex and the presence of mental disorders play an important role in FA among COPD patients. Our findings are in line with other studies which also associated higher age, female gender6,7 and the presence of depression, dementia or anxiety with a greater number of healthcare requests.1,3,8–11 Tobacco use reflects an interesting aspect, smokers show a lower degree of MF attendance. There is the possibility that MF attenders endeavor to make less use of primary care to avoid receiving anti-smoking counseling.12
In both profiles, patients who reside closer to out-of-hospital settings were observed to have a higher likelihood of being frequent attenders at these facilities. One explanation might possibly be a degree of perceived difficulty in accessing hospital services, which leads patients to seek greater support in out-of-hospital services.13 It should be mentioned that, in this study's healthcare area, there is just one tertiary hospital in a city and therefore in this context distance to hospital can be assimilated as rurality.
The main limitation is the exclusion of a substantial percentage of subjects for not meeting the spirometry criteria. We included solely those subjects that had a confirmed diagnosis – with available spirometry results – to avoid including subjects that might not have COPD. The use of cutpoints to assess FA could also be seen as a limitation. However, the cutpoints used are similar to those applied in previous studies.14,15 The information regarding comorbidities was obtained from the EMR and we cannot disregard some misclassification. Furthermore, the reason for the visit to the out-of-hospital setting could not be specified. Lastly, there are not studies with AUC information from other models therefore it is not possible to compare our values with those from other studies.
This study also has strengths. The inclusion of the whole population of patients allocated to a given health area ensures representativeness of the local population and serves to reduce patient selection bias. Also, a uniform data-collection system was applied. Data loss was zero since the databases are regularly updated. The follow-up period was long enough to allow for the occurrence of events of interest. Lastly, our study shows that the joint use of health information systems by experts affords an enormous potential for the generation of useful scientific evidence for clinical decision-making.
In conclusion, the profile of both FA groups (MF and EF) in out-of-hospital care attests to the complexity confronting the clinical and care management of COPD patients. Factors associated with FA may help identify certain groups of patients who, by reason of their chronicity and complexity, would benefit from actions which they are currently not receiving and on which the healthcare system should lay special stress.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approvalThis study protocol was reviewed and approved by the Santiago-Lugo Research Ethics Committee under registry code 2016/196.
Author's contributionsME López-Pardo: Conceptualization, Data curation, Formal analysis, Writing – original draft.
A Ruano-Ravina: Conceptualization, Methodology, Surpervision, Writing – review and editing.
L Valdés-Cuadrado: Conceptualization, Methodology, Writing – review and editing.
C Represas-Represas: Methodology, Writing – review and editing.
C Candal-Pedreira: Formal analysis, Writing – review and editing.
M Pérez-Ríos: Formal analysis, Writing – review and editing.
All authors have read and provided intellectual input to the manuscript.
All authors have approved the final version of the manuscript and take public responsibility of its content.
Conflict of interestNone declared.