Tuberculosis (TB) is still a public health issue that affects a large number of individuals and generates high healthcare costs.1–3 Moreover, hospital stays in patients with TB tend to be prolonged; over 15 days in most cases.2,3 In Spain, between 1999 and 2009, mean hospital stay was 14 days with a standard deviation of 12 days.3
Very few studies have been conducted in Spain to explain the reasons for these prolonged mean stays. The aim of this study was to analyze TB patients who were admitted to hospital for mean stays of longer than 15 days, and to evaluate the associated factors.
This was a retrospective observational study analyzing all patients admitted for TB between January 2005 and August 2012 in the Hospital General Universitario Reina Sofía, Murcia.
On the basis of data published by Thomas et al., 4 mean stay was considered prolonged if it was longer than 15 days.
The analysis included 165 patients. Mean patient age was 37.69 (14.42) years, 66% were men, 66% immigrants, 78.2% had pulmonary TB, 21.8% had extrapulmonary TB, and 22.4% presented complications during admission.
Mean stay of all TB patients was 21.94 (29.7) days, median 15 (IQR, 11–24) days, and longer than 15 days in 54.5% of patients. Mean stay of patients with pulmonary tuberculosis was 18 (12.21) days, median 14 days (IQR, 11–22).
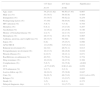
Table 1 shows the univariate analysis of factors associated with prolonged mean stay (≥15 days).
Univariate Analysis of Factors Associated With Mean Hospital Stay ≥15 Days.
| <15 days | ≥15 days | Significance | |
|---|---|---|---|
| N=75 | N=90 | ||
| Age, years | 34.25 (11.82) | 40.56 (17.43) | 0.007 |
| Male sex (%) | 53 (70.7) | 59 (65.6) | 0.484 |
| Immigration (%) | 53 (70.7) | 56 (62.2) | 0.254 |
| Predisposing factors (%) | 37 (50) | 58 (64.4) | 0.062 |
| HIV infection (%) | 5 (6.7) | 7 (7.8) | 0.784 |
| Homeless (%) | 6 (8.1) | 13 (14.4) | 0.207 |
| Alcoholism (%) | 12 (16.2) | 23 (25.6) | 0.146 |
| History of bronchial disease (%) | 2 (2.7) | 12 (13.3) | 0.015 |
| Hemoptysis (%) | 28 (37.3) | 16 (17.8) | 0.005 |
| Asthenia, anorexia, and weight loss (%) | 26 (34.7) | 54 (60) | 0.001 |
| Sepsis (%) | 6 (8) | 15 (16.7) | 0.096 |
| APACHE II | 1.6 (3.09) | 3.05 (3.8) | 0.012 |
| Bilateral involvement (%) | 24 (32) | 46 (51.1) | 0.013 |
| Extrapulmonary involvement (%) | 10 (13.3) | 26 (28.9) | 0.016 |
| Pleural effusion (%) | 8 (10.7) | 19 (21.1) | 0.071 |
| Bacilliferous on admission (%) | 40 (52) | 51 (58.4) | 0.754 |
| Drug resistance (%) | 10 (19.2) | 18 (27.3) | 0.308 |
| Complications (%) | 5 (6.7) | 32 (35.6) | <0.001 |
| CCI | −0.77 (0.95) | 0.96 (3.44) | 0.058 |
| UCI admission (%) | 2 (2.7) | 2 (2.2) | 0.853 |
| Lost-to-follow-up (%) | 18 (24.3) | 35 (38.9) | 0.047 |
| Cure (%) | 54 (91.5) | 49 (74.2) | 0.011 (of n=125) |
| Relapse (%) | 5 (9.3) | 13 (19.7) | 0.069 |
| Death (%) | 3 (5) | 6 (9.1) | 0.373 |
| Delayed diagnosis, days | 1 (3.7) | 3.6 (7.27) | 0.01 |
CCI: Charlson comorbidity index; ICU: intensive care unit.
Variables associated independently with prolonged mean stay in the logistic regression analysis were delayed diagnosis (health system delay) beyond the fourth day (OR 17.94; 95% CI 3.47–92.79; P=.001), complications during admission (OR 7.87; 95% CI 2.63–23.8; P<.005), history of bronchial disease (OR 6.21; 95% CI 1.17–33.3; P=.031) and weight loss, weakness/asthenia and anorexia at time of presentation (OR 3.89; 95% CI 1.83–8.26; P<.005) or bilateral involvement (OR 2.64; 95% CI 1.25–5.58; P=.011).
The most important factor associated with prolonged stay was delayed diagnosis, to the extent that a delay beyond the fourth day increased by 18-fold the probability of stays longer than 15 days.
Delayed diagnosis, moreover, helps keep tuberculosis endemic,5–7 and it can also increase morbidity and mortality,8 and extend hospital stay,5–9 underlining the importance of early diagnosis and the implementation of preventive measures.
Factors that influence this delay are wide-ranging, but, as we found in our study, advanced age, extrapulmonary involvement, disease site other than the upper lobes, and a negative Ziehl sputum test are determinant factors.6–8
Complications during hospitalization have also been described as a key factor in prolonging mean hospital stay.8,10,11 Complications most commonly observed were toxicities associated with anti-tuberculous drugs (mainly liver involvement), and the need for major surgery in patients with extrapulmonary TB.
Other factors associated with prolonged stay were a history of bronchial disease (risk factor for developing TB and complications1,8,10), while bilateral involvement with asthenia, anorexia, and weight loss are associated with more severe disease,1 leading to a longer mean stay.
It is interesting to point out that a hospital stay of longer than 15 days is not an isolated problem in our center; it also occurs in other Spanish hospitals. Indeed, the analysis of the minimum basic data set of discharges from Internal Medicine departments of the Spanish National Health System in 2005–2010 showed that the mean stay was 18.7 days (range 19–44), with 17.8 (SD 19.3) days for patients with extrapulmonary tuberculosis, 18 (SD 22.25) days for patients with pulmonary tuberculosis, and 24.7 (SD 22) days for patients with disseminated disease.3
One of the main reasons for keeping patients hospitalized for such long periods is to avoid propagation of the TB. However, the risk of propagation is not reduced by hospitalization, since exposure occurs before diagnosis, and the risk of contagion falls dramatically after treatment is started.12–14 In a study performed in New York, up to 40% of hospitalizations were found to be inappropriate on this basis.4
Hospitalization, and particularly long hospitalization, is not always necessary.4,14 It is generally an inefficient use of resources and probably up to 20%–40% of admissions among TB patients could be avoided.4
In conclusion, most patients admitted with TB have a prolonged mean stay (≥15 days) associated with delayed diagnosis, asthenia, anorexia, and weight loss, previous bronchial disease, bilateral involvement, and complications during admission.
The most important factor for prolonging mean hospital stay in these patients was delayed diagnosis, so it is essential that the optimal measures for avoiding this delay are implemented, including improved TB education for physicians and the general public (in order to increase the diagnostic suspicion), and better access to the health system. We also believe that a large number of TB patients could benefit from outpatient treatment, reducing the length of hospital stay, or even avoiding hospitalization altogether. This would require, most importantly, the use of standardized protocols, improved health education among patients and family members about isolation measures in the home and treatment compliance, and multidisciplinary teams for supervised outpatient treatment or directly observed therapy.15
Please cite this article as: Sánchez-Rojas MC, Pérez EM, Pérez ÁM, Cifuentes SV, Villalba EG, Campoy MP, et al. Factores asociados con estancia media prolongada en pacientes ingresados por tuberculosis. Arch Bronconeumol. 2017;53:409–410.