Intravascular lipoma is defined as a lipoma arising in the media layer of blood vessels with low adipocyte content; an extravascular or extraluminal lipoma may be formed by invagination of adjacent fatty tissue. Only 9 cases of lipoma in the vascular wall have been described.1
We present the case of a lipoma located in the left subclavian artery. We have found no similar cases in the literature.
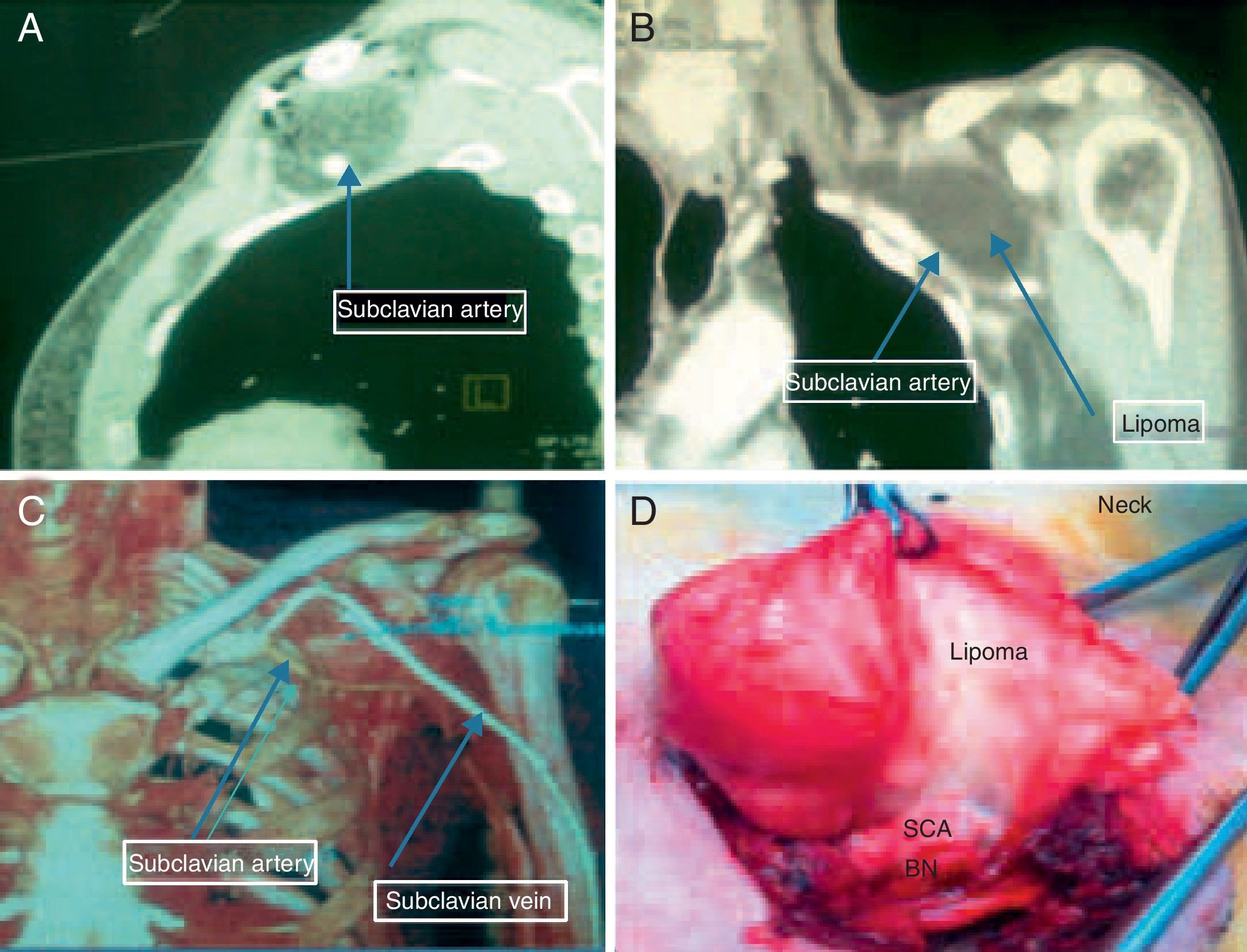
A 65-year-old male was admitted due to a mass in the region of the left subclavian artery. Physical examination showed a deep mass, 6mm in size, along the subclavian artery with no neurological or vascular deterioration. Sonography and computed tomography (CT) of the chest (Fig. 1A–C) revealed a well-defined mass that was thought to possibly be an extremely rare subclavian lipoma. There was extensive contact along the subclavian artery but no intravascular mass. The tumor was excised via an incision in subclavian region, after being safely separated from the adjacent subclavian artery and vein and brachial nerve structures (Fig. 1D). The subclavian vein sustained a minimal injury that could be rapidly repaired. The patient's progress was incident-free. Histopathological examination revealed mature adipocytes.
(A) Chest CT showing a hypodense mass in the subclavian region (transversal projection). (B) Sagittal chest CT showing slight contact of mass with left subclavian artery. (C) CT reconstruction showing subclavian vein and artery separated by the lipoma. (D) Preoperative image of lipoma with persistent adherence to the subclavian artery. BN: brachial nerve; SCA; subclavian artery; SCV: subclavian vein.
Lipomas are very uncommon primary vascular tumors arising in venous walls, particularly in the inferior vena cava, and are found in 0.5% of abdominal CT examinations.2
Extravascular lipomas are very rare, and intravascular lipomas are extraordinarily rare. A hypothesis to explain the formation of these lipomas has been proposed: the tumor may arise in the vascular wall or in the perivascular adipose tissue. When the lipoma arises in the vascular wall, intravascular growth may be seen even when the vascular media layer is underdeveloped and contains few adipose cells.3 This suggests that our patient's tumor arose in the perivascular tissue and subsequently penetrated the artery via mechanical intrusion or invagination rather than by infiltration of the vascular wall.
Most vascular lipomas are asymptomatic and are revealed on incidental CT or magnetic resonance imaging (MRI). Symptomatic tumors may cause thrombosis or venous occlusion.4
Although the presence of a lipoma may be confirmed by sonography, the magnitude and depth of the subclavian lesions cannot be appropriately assessed with this technique. Both CT and MRI are useful for the evaluation of subclavian lipomas. Advocates of MRI believe that it provides reliable confirmation of the adipose character of the mass and a more accurate definition of the magnitude of the lesion and its relationship with surrounding structures. We, however, agree with the CT defenders who claim that most of the clinically relevant information on most lesions can be accessed by CT just as clearly as with MRI, but CT is preferable for reasons of cost, availability and ease in obtaining images.
Differential diagnosis includes angiomyolipoma, poorly encapsulated, containing mature adipocytes and small vessels with heterotopic calcifications, cavernous hemangioma, a vascular mass with small serpiginous vessels and phleboliths, cystic hemangioma, mixed-fibrous tumors and lipomatous hemangiopericytoma.5
Symptomatic lipoma or suspected malignancy are indications for surgical intervention.
Lipomas located in atypical sites are not easy to operate. Careful planning is necessary and the patient must be referred to a cardiothoracic surgeon. Adverse consequences of treatment, such as vascular lesions in a conscious patient or injuries caused by an inexperienced surgeon must be avoided.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: El Hammoumi M, Taberkanet M, Kabiri EH. Lipoma extravascular de la arteria subclavia. Arch Bronconeumol. 2014;50:562–563.