Amyloidosis is a disease of unknown origin that consists of abnormal extracellular deposit of amyloid material in various organs. It is usually classified as either primary or secondary, and localized or systemic, depending on which organs are involved. Primary tracheobronchial amyloidosis (TBA) is considered a variant of localized pulmonary amyloidosis.
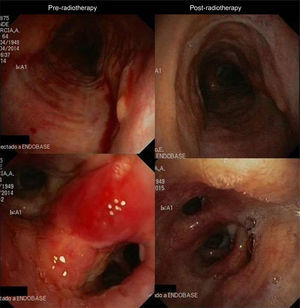
We report the case of a 65-year-old man, former smoker (18 pack-years), referred to our hospital due to hemoptysis. Baseline examination showed modified Medical Research Council (MMRC) dyspnea scale 2, and a history of orthopnea of several months. Computed tomography (CT) showed diffuse circumferential thickening of the tracheal wall, and main, lobar and segmentary bronchi, with no pulmonary parenchymal involvement. Fiberoptic bronchoscopy showed partial tracheal collapse due to excessive mobility and loss of structure of the membranous wall, with fragile mucosa and whitish plaques. The main, lobar and segmentary carina were widened and misshapen (Fig. 1). Bronchial biopsy was indicative of amyloidosis. Lung function tests showed FEV1 2500 cc (81%), FVC 3430 cc (88%), FEV1/FVC 73. In view of the diffuse involvement of the disease, endoscopic treatment with laser and/or placement of endobronchial stents was ruled out. In the absence of evidence of systemic involvement, external beam radiation therapy (EBR) to a total dose of 24Gy in 12 fractions of 2Gy was proposed.
After completion of treatment, clinical improvement was observed and the patient was able to tolerate a supine decubitus position, with MMRC dyspnea scale 1, lung function test results FEV1 3210 cc [101%], FVC 4210 cc [104%], FEV1/FVC 76. Endoscopy showed mild stenosis of the left upper and lower lobe bronchi, due to mucosal thickening (Fig. 1). Side effects included spells of supraventricular tachycardia managed with medication, and grade 1 esophagitis. The patient is currently clinically and functionally stable, 1 year after treatment.
BTA is an uncommon variant of amyloidosis that affects the lower respiratory tract. Amyloid deposits appear on the airway walls as polypoid nodules and/or submucosal plaques. It mainly affects middle-aged men. Clinical manifestations are non-specific: cough, wheezing, dyspnea, hemoptysis, etc.1 Chest CT provides information on the involvement and extent of the disease, revealing different degrees of involvement of the respiratory tract walls, which appear thickened with narrowing of the lumen. Lung function tests often show an obstructive pattern, but when the involvement is distal, results may be normal. Diagnosis is obtained from bronchial biopsy.1
Evidence regarding treatment is limited and based on endoscopic recanalization techniques using CO2 and Nd:YAG lasers, cryosurgery, or the placement of endobronchial stents.2 However, the benefits in cases of diffuse involvement are small, and disease progression is not halted, so repeated resections with the attendant risk of bleeding are required. EBR is a promising alternative in the treatment of diffuse disease, and long term benefits have been reported. This technique has been used successfully in benign disease, with doses of 2Gy providing an anti-inflammatory effect.3 This treatment was first described in 1998 by Kurrus et al.4 Since then, evidence remains limited, but doses of 20Gy administered in a fractionated manner cause a radiological, endoscopic and functional response, the effects of which are maintained for about 2 years.5 Our patient received treatment at the standard dose described in the literature, showing radiological, functional and endoscopic improvement that has been maintained to date. Although the dose has not yet been well defined, most patients undergoing this technique had mild side effects.5
Please cite this article as: Pacheco VA, Crespo EL, Zurita AJW, Rubio TM. Amiloidosis traqueobronquial difusa: uso de radioterapia local externa como modalidad de tratamiento. Arch Bronconeumol. 2015;51:607–608.