Gasometric analysis of an arterial blood sample provides valuable information on respiratory function, both in terms of gas exchange and acid–base balance (pH).1 The puncture to obtain this arterial blood sample is uncomfortable and painful for patients to varying degrees.2,3 There are recommendations that consider the administration of subcutaneous local anesthetics as a possible gold standard for the management of this pain.4–6 Traditionally, the infiltration of these drugs (lidocaine, mepivacaine) is mostly not performed by nurses.1 In addition, unfamiliarity with the procedure or lack of time are known barriers to its use.7,8
The aim of this study was to find factors that could explain the administration of local anesthetics of the amide group for the management of pain produced by direct arterial puncture for blood gas analysis by nursing professionals in different clinical settings in a European region (Castilla-La Mancha).
A cross-sectional multicenter analytical multicenter study was conducted in response to the proposed objective. An electronic form was used as an instrument to collect the variables of interest. This form was sent through the corporate mail of the Public Health Service to all those with an active nursing profile, with a new reminder for participation one month after the preliminary call. In addition to consenting to participate, only nurses who had ever performed an arterial puncture for blood gas analysis were selected. The form (Supplementary material S1) was available to the selected population for 4 months (August–November 2022). An approval report was obtained from the Clinical Research Ethics Committee of the center where the study was designed with code 12/2022 (Supplementary material S2).
Based on a population of 10,482 nurses and a literature estimate of 23% of nurses routinely using local anesthetics,1,7–10 we calculated a sample size of 528 participants. Qualitative variables were described using frequencies and percentages, and quantitative variables were described using medians and 1st and 3rd quartiles. The χ2 test and the Wilcoxon–Mann–Whitney test were used for hypothesis testing. A multivariate explanatory model was generated by binary logistic regression, using odds ratio (OR) as a measure of the magnitude of the association and the predicted probabilities were presented by calculating the AUCROC, sensitivity and specificity. A statistical significance level of p<0.05 was set for all contrasts. The open-source software Jamovi based on R software was used for these analyses.
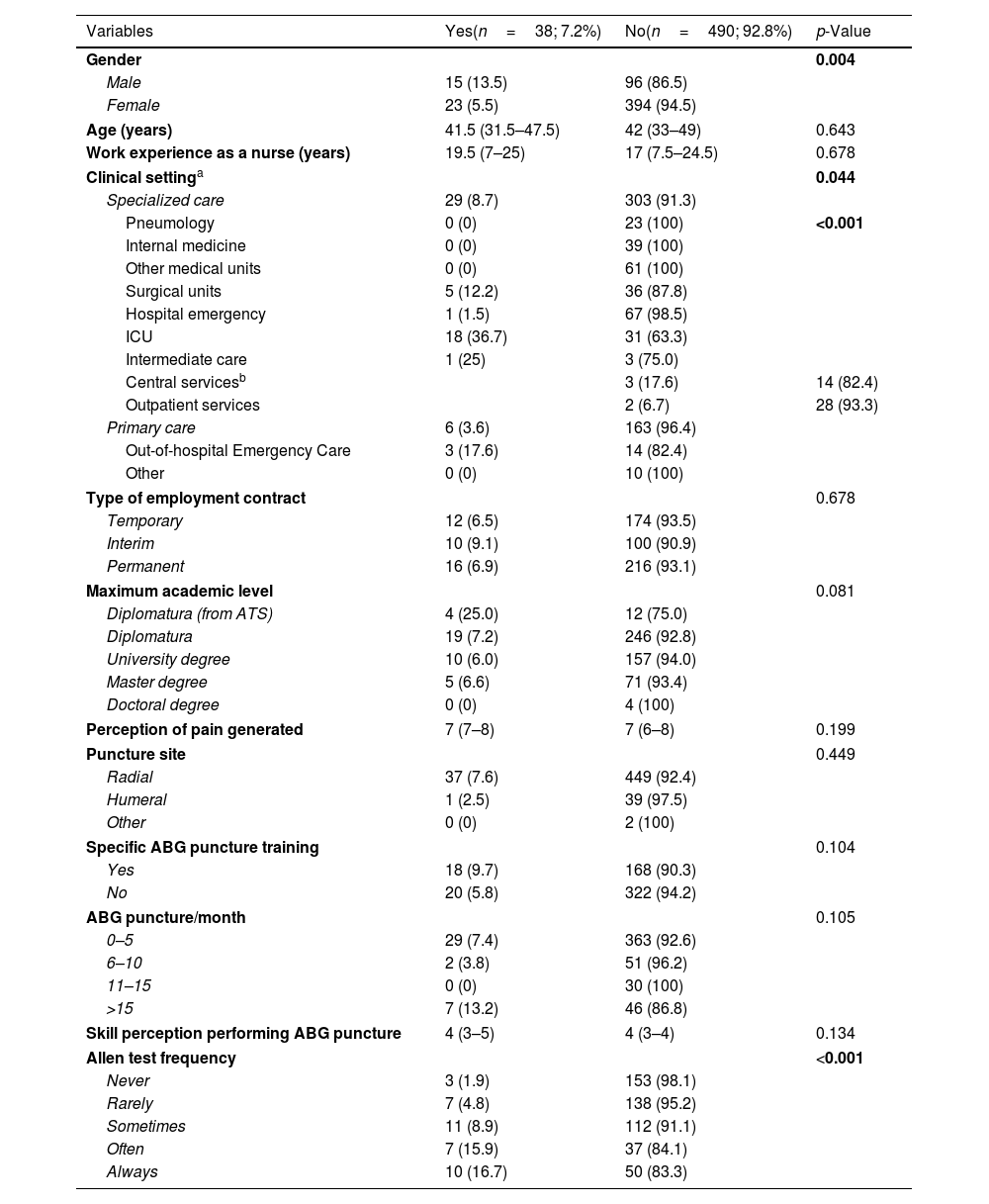
From a total of 10,482 questionnaires sent finally 528 nurses participated in this study, of whom only 7.2% routinely used local anesthetics prior to performing direct arterial puncture for blood gases. Seventy-nine percent were female with a median age of 42 years. Sociodemographic, professional, and technique-related variables according to local anesthetic use are shown in Table 1. Significant differences were found between the use of anesthetics and the following socio-demographic factors: gender, clinical setting, and type of specialized care unit. Male professionals were more likely to use this intervention (15 (13.5%) vs. 23 (5.5%); p=0.004). Regarding the clinical setting in which the research participants work as nurses, differences were found, with a higher proportion of use of subcutaneous local anesthetics in Out-of-hospital Emergency Care, 3 (17.6%), followed by specialized care, 29 (8.7%) (p=0.044). The last significant socio-work variable was the type of work unit. The intensive care unit was the department where there was a higher proportion of nurses using this intervention, 18 (36.7%) (p>0.001). In addition, differences were observed in the use of subcutaneous anesthetics according to the frequency of the Allen test (p<0.001). Nurses who reported using the Allen test always, 10 (16.7%) and almost always, 7 (15.9%) were more likely to perform this type of procedure.
Sociodemographic variables and specific characteristics of gasometric puncture after subcutaneous administration of local anesthetics (lidocaine, mepivacaine).
| Variables | Yes(n=38; 7.2%) | No(n=490; 92.8%) | p-Value |
|---|---|---|---|
| Gender | 0.004 | ||
| Male | 15 (13.5) | 96 (86.5) | |
| Female | 23 (5.5) | 394 (94.5) | |
| Age (years) | 41.5 (31.5–47.5) | 42 (33–49) | 0.643 |
| Work experience as a nurse (years) | 19.5 (7–25) | 17 (7.5–24.5) | 0.678 |
| Clinical settinga | 0.044 | ||
| Specialized care | 29 (8.7) | 303 (91.3) | |
| Pneumology | 0 (0) | 23 (100) | <0.001 |
| Internal medicine | 0 (0) | 39 (100) | |
| Other medical units | 0 (0) | 61 (100) | |
| Surgical units | 5 (12.2) | 36 (87.8) | |
| Hospital emergency | 1 (1.5) | 67 (98.5) | |
| ICU | 18 (36.7) | 31 (63.3) | |
| Intermediate care | 1 (25) | 3 (75.0) | |
| Central servicesb | 3 (17.6) | 14 (82.4) | |
| Outpatient services | 2 (6.7) | 28 (93.3) | |
| Primary care | 6 (3.6) | 163 (96.4) | |
| Out-of-hospital Emergency Care | 3 (17.6) | 14 (82.4) | |
| Other | 0 (0) | 10 (100) | |
| Type of employment contract | 0.678 | ||
| Temporary | 12 (6.5) | 174 (93.5) | |
| Interim | 10 (9.1) | 100 (90.9) | |
| Permanent | 16 (6.9) | 216 (93.1) | |
| Maximum academic level | 0.081 | ||
| Diplomatura (from ATS) | 4 (25.0) | 12 (75.0) | |
| Diplomatura | 19 (7.2) | 246 (92.8) | |
| University degree | 10 (6.0) | 157 (94.0) | |
| Master degree | 5 (6.6) | 71 (93.4) | |
| Doctoral degree | 0 (0) | 4 (100) | |
| Perception of pain generated | 7 (7–8) | 7 (6–8) | 0.199 |
| Puncture site | 0.449 | ||
| Radial | 37 (7.6) | 449 (92.4) | |
| Humeral | 1 (2.5) | 39 (97.5) | |
| Other | 0 (0) | 2 (100) | |
| Specific ABG puncture training | 0.104 | ||
| Yes | 18 (9.7) | 168 (90.3) | |
| No | 20 (5.8) | 322 (94.2) | |
| ABG puncture/month | 0.105 | ||
| 0–5 | 29 (7.4) | 363 (92.6) | |
| 6–10 | 2 (3.8) | 51 (96.2) | |
| 11–15 | 0 (0) | 30 (100) | |
| >15 | 7 (13.2) | 46 (86.8) | |
| Skill perception performing ABG puncture | 4 (3–5) | 4 (3–4) | 0.134 |
| Allen test frequency | <0.001 | ||
| Never | 3 (1.9) | 153 (98.1) | |
| Rarely | 7 (4.8) | 138 (95.2) | |
| Sometimes | 11 (8.9) | 112 (91.1) | |
| Often | 7 (15.9) | 37 (84.1) | |
| Always | 10 (16.7) | 50 (83.3) | |
Qualitative variables: frequency (percentage). Quantitative variables: median (Q1–Q3).
Hypothesis testing. For quantitative variables: Wilcoxon-Mann–Whitney test. For qualitative variables: χ2 test.
Values in bold are statistically significant (p<0.05).
ABG: arterial blood gas; ATS: nursing studies prior to the creation of the university diploma.
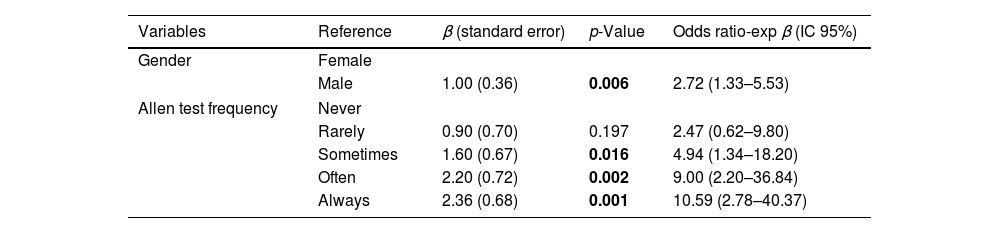
Table 2 shows the multivariate explanatory model for the use of subcutaneous anesthetic injections such as lidocaine or mepivacaine to reduce pain caused by direct arterial puncture for blood gases. In this case, the variables included were gender and frequency of use of the Allen test. In terms of gender, men were more likely to use anesthetics than women. The OR obtained was 2.72 [1.33–5.53; 95%CI]. Regarding nurses who do not use the Allen test, the odds of using subcutaneous anesthetics were statistically significant in those who reported performing this test: sometimes OR 4.94 [1.34–18.20; 95% CI], often OR 9.00 [2.20–36.84; 95% CI], and always OR 10.59 [2.78–40.37; 95% CI]. And finally, in terms of discriminatory and predictive ability of this model, the AUCROC was 0.740 [0.665–0.814; 95%CI], the sensitivity was 86.84% and the specificity was 53.67%.
Explanatory model, discriminative capacity and validity indicators for the use of the pain reduction intervention: subcutaneous injection of local anesthetics (lidocaine, mepivacaine).
| Variables | Reference | β (standard error) | p-Value | Odds ratio-exp β (IC 95%) |
|---|---|---|---|---|
| Gender | Female | |||
| Male | 1.00 (0.36) | 0.006 | 2.72 (1.33–5.53) | |
| Allen test frequency | Never | |||
| Rarely | 0.90 (0.70) | 0.197 | 2.47 (0.62–9.80) | |
| Sometimes | 1.60 (0.67) | 0.016 | 4.94 (1.34–18.20) | |
| Often | 2.20 (0.72) | 0.002 | 9.00 (2.20–36.84) | |
| Always | 2.36 (0.68) | 0.001 | 10.59 (2.78–40.37) | |
| AUC ROC | CI 95% | p-Value | Sensitivity | Specificity |
|---|---|---|---|---|
| 0.740 | 0.665–0.814 | <0.001 | 86.84% | 53.67% |
Model information: R2 (Nagelkerke)=0.127. χ2=27,832 p-value=<0.001. Hosmer–Lemeshow test p-value=0.666.
Exp β: beta exponential.
Null hypothesis: AUCROC=0.5.
Other studies conducted in settings like ours have also evaluated some factors addressed in our research. For example, regarding the frequency of anesthetic infiltration according to specialized care unit, the underuse in pneumology services is noteworthy. Although the overall prevalence is low in all these studies, the use in pneumology stands out in these studies7 compared to other units such as emergency departments.8 In contrast, ICUs have the highest proportion of anesthetic use. Many of the arterial punctures performed by these nurses are for cannulation of arterial catheters, a technique that is even more painful than direct puncture. It is estimated that 36% of patients treated in the ICU have an established arterial line.11 Therefore, the use of anesthesia is an established practice even for direct arterial punctures for gasometric analysis. It is necessary to investigate in the future the barriers to the use of amide-type local anesthetics and the non-compliance with recommendations such as those proposed by scientific societies4 or the WHO.12
Gender was shown to be a differential factor in our study, both in the crude analysis and in the adjusted analysis. Despite the fact that the number of female participants was much higher than the number of male participants, these data are consistent with published data on registered nurses collected by the National Institute of Statistics.13 Other studies have also reported low rates of local anesthetic use by women, and this is a constant finding over time, which means that our results may be generalizable.14 The scientific literature indicates that health care may be provided differently depending on the gender of the patients, but also of the clinicians themselves.15 Further studies are needed to analyze in detail these gender differences in the use of local anesthetics for this purpose.
On the other hand, the almost direct association between the frequency of performing the Allen test and the use of local anesthetics is surprising. The WHO recommends the use of this test as good practice to ensure the presence of collateral blood flow.12 However, there are arguments against the modified Allen test because of its low validity compared to other methods such as plethysmography or the use of ultrasound.16,17 To the best of our knowledge, many of the training documents continue to recommend the use of the Allen test4,12 as well as local anesthetics, so perhaps those nurses who follow these guidelines prefer to perform both procedures together. In any case, as with the previous findings regarding nurse gender, future research is needed to clarify this association with the use of local anesthetics.
In conclusion, this study demonstrates in a well-representative sample that gender, clinical setting, type of specialized care unit, and frequency of performing the Allen test are associated with the use of injectable local anesthetics as an intervention to reduce pain caused by arterial puncture for blood gases.
Authors’ contributions (CRediT)Conceptualization, JAMA and IZG; data curation, JAMA, RSG and IOS; formal analysis, JAMA and IZG; investigation, JAMA and IZG; methodology, JAMA, IZG and IOS; project administration, JAMA, IZG and SGA; resources, JAMA and PPM; software, JAMA, RSG, SGA, IOS; supervision, RSG and PPM; validation, JAMA, IZG and PPM; visualization, JAMA, IZG and RSG; writing—original draft, JAMA, IZG, PPM; and IOS; writing—review and editing, JAMA, IZG, RSG, SGA and IOS. All authors have read and agreed to the published version of the manuscript.
Funding sourcesThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors state that they have no conflict of interests.
We would like to thank all the nurses who participated in this study, the General Directorate of Care of SESCAM and the Research Support Unit of “Gerencia de Área Integrada de Salud de Talavera de la Reina”.