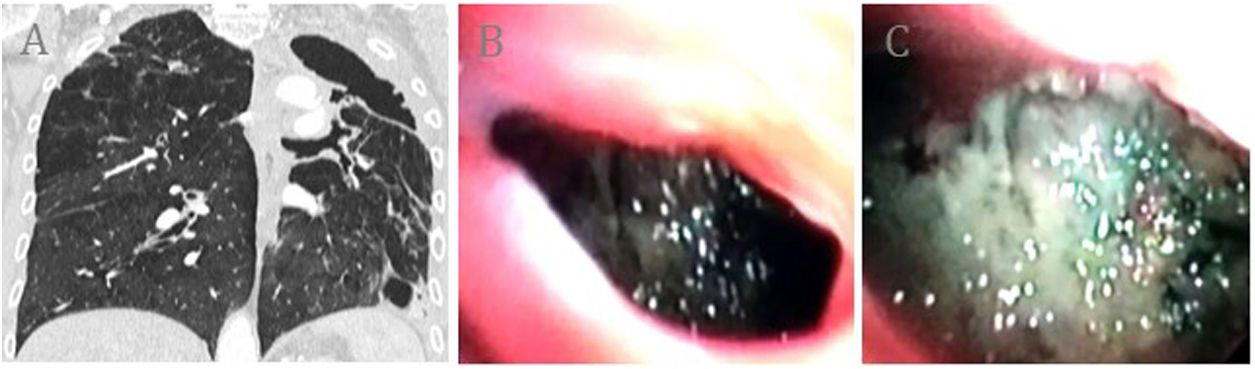
Our patient was a 77-year-old man, 40-pack-year former smoker, with an incidental finding of a cavitated lesion in the left upper lobe on X-ray and CT (Fig. 1A). Fiberoptic bronchoscopy was used to access the cavitation, which showed irregular walls and isolated necrotic remains (Fig. 1B, C). Biopsies of the lesion showed signs of inflammation, while cytology and microbiology studies of bronchial aspirate and lavage were negative. Autoimmune disease was ruled out with history, physical examination, and laboratory tests. PET-CT confirmed a chronic appearance and a residual cavitated lesion was diagnosed. No changes were observed in a subsequent 2-year follow-up.
(A) Pulmonary cavity in the left upper lobe associated with pleural thickening, loss of left lung volume, bronchiectasis, and emphysema. The left upper lobar bronchus that connects with the cavity through the apical segment can be observed. (B) Subsegmental division of the left apical bronchus containing the cavity. (C) Visualization of the cavity containing necrotic and inflammatory mucosa.
Lung cavities are air-filled spaces with a wall thickness greater than 4mm that require a wide differential diagnosis based on different examinations that do not offer direct vision, such as sputum analysis, fiberoptic bronchoscopy, targeted biopsies, and imaging tests.1 It is exceptional to be able to access and view the cavity, as in our case, and the collection of direct samples excluding the major etiologies helped avoid more invasive techniques or surgery and facilitated follow-up with a lower risk of missing serious disease.1,2
FundingWe acknowledge that there are no primary funders or grants for this research.