Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) stands as the recommended technique for sampling mediastinal lymph nodes and staging lung cancer.1,2 While it exhibits high sensitivity and specificity in diagnosing and staging primary lung cancer, the efficacy of EBUS-TBNA in identifying other etiologies such as lymphoproliferative diseases is limited. In such cases, larger tissue samples are often required, leading to more invasive procedures such as mediastinoscopy.3 Transbronchial lung cryobiopsy has emerged as a valuable method for tissue sampling, particularly in cases of interstitial lung diseases.4 In parallel with this clinical application, some groups have documented the use of small bore cryoprobes with EBUS bronchoscopes, in a procedure commonly designated as EBUS-guided transbronchial mediastinal cryobiopsy (cryoEBUS). Preliminary data suggests that this procedure can effectively and safely increase the diagnostic yield, particularly in the specific setting of benign and lymphoproliferative disorders.5–7
We present a retrospective observational study conducted at Instituto Português de Oncologia de Coimbra aimed to assess the diagnostic yield, feasibility, and safety of cryoEBUS in patients with mediastinal lesions.
All EBUS procedures were performed under general intravenous anesthesia with secured airway through laryngeal mask or endotracheal tube. After identifying the appropriate lymph node using an EBUS bronchoscope (BF-UC190F, Olympus), a conventional EBUS-TBNA was performed using a 22-gauge needle (NA-U401SX; Olympus Medical Systems or SonoTip® EBUS Pro Medi-Globe). To enable sequential cryobiopsy, a second puncture was made immediately after the initial TBNA, targeting the proximal border of the lymph node. The goal was to rupture the lymph node capsule and create a tunnel for seamless introduction of the 1.1mm cryoprobe (Erbecryo 20402-401, Tübingen, Germany). Before inserting the cryoprobe, the echogenic needle trace, typically seen as a hyperechoic line within the lymph node on ultrasound, was used as a reference point to guide the cryoprobe placement. After the introduction of the 1.1mm cryoprobe a freeze cycle of 3–4s was applied. Samples were subsequently retrieved en-block with the EBUS bronchoscope and were then thawed in saline and fixed in formalin. On average, 3 criobiopsies were obtained per lymph node approached. All participants were admitted as in-patients for a period of 24h after the procedure. A subsequent follow-up at week 4 after the procedure was performed routinely to rule out late onset complications.
A total of 27 patients were selected for cryoEBUS. However, the procedure was not performed in two patients. In one case, the decision to halt the procedure was due to the lymph node characteristics (grade III vascular pattern).8 In the second case, grade 2 bleeding9 occurred after EBUS-TBNA, and consequently we didn’t proceed with the cryoEBUS, as we were concerned that it would exacerbate the bleeding. The remaining 25 patients underwent cryoEBUS. The mean age of the patients who underwent cryoEBUS was 54±13 years old, with the majority being male (n=18, 72%). Most patients had no smoking habits (n=21, 84%). All EBUS procedures were performed for diagnostic purposes. Prior to cryoEBUS, some patients had already undergone other procedures to achieve a diagnosis with negative or inconclusive results: CT-guided percutaneous transthoracic needle biopsy (n=1), EBUS (n=7, 28%), esophageal ultrasound with ultrasound bronchoscope (EUS-B) (n=4, 16%).
Cryobiopsies were predominantly performed on station 7 (n=11), station 11L (n=12), station 11R (n=3), station 4R (n=2) and, in one patient, cryobiopsy was performed on a central mass. Minor bleeding (grade 1)9 was observed in 3 patients (8.5%) that resolved with simple suction. No major adverse events and no late onset complications were observed.
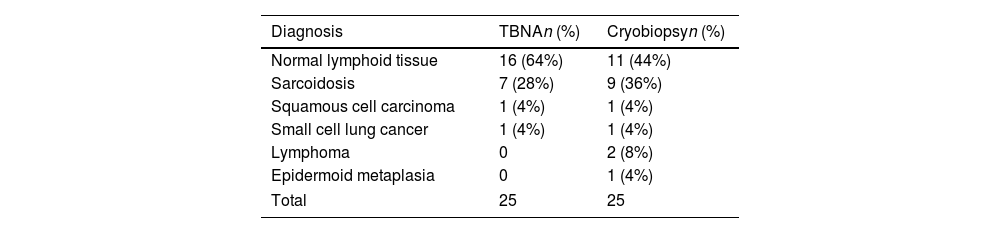
Histopathological results of both the EBUS-TBNA and cryo-EBUS are presented in Table 1. Both procedures performed equally well for malignancy whereas the cryobiopsy samples showed slightly higher sensitivity for the diagnosis of sarcoidosis and lymphoma. In this later scenario, one patient underwent subsequent confirmatory mediastinoscopy that was consistent with the diagnosis of marginal zone lymphoma, fully overlapping the information obtained by cryobiopsy.
CryoEBUS has emerged as a promising technique for obtaining larger samples from mediastinal lesions. This may be important, especially in lymphoproliferative and granulomatous diseases, where EBUS-TBNA has a lower diagnostic yield and more invasive procedures are frequently needed.1 This study involved 25 cryoEBUS procedures, all for diagnostic purposes. Prior to cryoEBUS, some patients had already undergone other procedures with negative or inconclusive results. However, selection criteria for cryoEBUS are lacking. Our patients were selected for cryoEBUS after undergoing other procedures without conclusive results or patients with a high suspicion of lymphoproliferative disease, in which the indication for EBUS-TBNA is controversial.1 In a significant number of cases (n=14, 56%), cryobiopsy was able to clarify the diagnosis without any major complications, thus preventing other more invasive procedures. Interestingly, in our series, one diagnosis of marginal zone lymphoma obtained by cryobiopsy was confirmed by mediastinoscopy (with no further details retrieved by this more invasive procedure). Our findings are in line with those from other studies, reporting cryoEBUS as a feasible and safe technique with a high diagnostic yield. However, the technique used in our patients presented some differences from most previously published data in which a SonoTip®TopGain: Medi-Globe needle or a high-frequency needle knife were used.5–7 Here we report the possibility to perform criobiopsy in sequential fashion after conventional EBUS-TBNA with the simple beveled 22G needle, as recently published by other groups.10
Our results support that cryoEBUS may be a valuable tool and a safe procedure aiding in the diagnosis of mediastinal lesions while preventing more invasive procedures. Further studies are needed to compare the diagnostic yield of cryoEBUS, EBUS-TBNA, and mediastinoscopy.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.
Artificial intelligence involvementThe authors declare that no artificial intelligence software or tool was used in the development of this article.