Community acquired pneumonia (CAP) is a highly prevalent pathology whose etiology is determined by the characteristics of the geographic region, the causative agent and the patient. The study of these features is essential for a proper therapeutic approach. Our aim was to study the changes of the causative agent of CAP brought about by the influence of seasonal and climatic changes in our geographic area.
Patients and methodsA prospective and longitudinal study of patients admitted with CAP was done from January 2006 to December 2009. We analyzed demographic data, comorbidities, severity, etiologic agent, complications and mortality. We correlated mean temperature and mean cumulative rainfall for each season with Streptococcus pneumoniae and Legionella pneumophila. Statistical analyses included: Chi squared test, Student's t-test for independent samples, variance analysis and Spearman's correlation.
ResultsWe included 243 patients, 64.6% men and 54.7% over the age of 65. The highest incidence of CAP was in the winter. S. pneumoniae was the most common causative agent for all seasons except in summer when the main agent was L. pneumophila. We observed a significant correlation between the lowest seasonal average temperature and pneumococcal etiology of CAP; inversely, with higher temperatures, L. pneumophila was more common. No etiological differences were found by season when related with environmental humidity.
ConclusionsIn our area, S. pneumoniae was the most common etiological agent in winter with low temperatures; in summer, with high temperatures, the most frequent was L. pneumophila.
La neumonía adquirida en la comunidad (NAC) es una patología muy prevalente cuya etiología viene dada por las características de la región geográfica y del paciente. El estudio de cada una de ellas es fundamental para su correcto abordaje terapéutico. Nos propusimos estudiar los cambios del agente causal de la NAC en función de la estacionalidad y la influencia de los cambios climáticos de nuestra área geográfica.
Pacientes y métodoEstudio prospectivo longitudinal de pacientes consecutivos ingresados por NAC desde enero de 2006 a diciembre de 2009. Analizamos datos sociodemográficos, comorbilidad, gravedad, agente etiológico, complicaciones y mortalidad. Correlacionamos la temperatura media y la precipitación acumulada media estacional para S. pneumoniae y Legionella pneumophila en cada estación del año. Análisis estadístico: Chi cuadrado, t de Student para muestras independientes, análisis de la varianza y correlación de Spearman.
ResultadosIncluimos 243 pacientes, 64.6% hombres y 54.7% mayores de 65 años. La mayor incidencia de NAC fue en invierno. Streptococcus pneumoniae fue el agente causal más frecuente en todas las estaciones del año a excepción del verano, que fue Legionella pneumophila. Observamos una correlación significativa entre la menor temperatura media estacional y la etiología neumocócica y a la inversa cuando el agente causal fue Legionella pneumophila. Sin embargo, no encontramos diferencias etiológicas por estaciones en relación con la humedad ambiental.
ConclusionesEn nuestra área, Streptococcus pneumoniae es el agente etiológico más frecuente en invierno con bajas temperaturas mientras que en verano, con altas temperaturas, es Legionella pneumophila.
Community-acquired pneumonia (CAP) is an illness of great epidemiological significance which remains a major cause of morbidity and mortality throughout the world, despite the treatments administered. Prospective population-based studies show an annual incidence of between 5% and 11% of the adult population,1 with an annual rate of around 1.62 per 100000 inhabitants.2 In this respect CAP is an illness whose incidence is high, but varies in accordance with time of year and geographical region, for which reason it is necessary to be able to determine not only its incidence and morbidity–mortality, but also the extent of seasonal variation, as this might well impinge upon the management of certain health-care resources. Nevertheless, despite the importance of seasonal factors in respiratory infection, most research studies have focused their attention on the analysis of seasonal variation in relation to Influenza virus infection rather than on bacteriological pathogens.3 Furthermore, very few studies have explored the possible relationship between climatological variations and the etiology of CAP. For this reason, it may be appropriate to analyze seasonal factors in the different etiology of CAP, and to determine whether climatological variations, within a particular season can have an impact on the etiological agent of CAP. The aim of our present study is to determine the extent to which the season of the year and climatological alterations within a single season can affect the variability of CAP etiology.
Patients and MethodsWe carried out a prospective, longitudinal and observational study of adult patients admitted consecutively for CAP to the Pulmonological Service of the Dr Peset University Hospital in Valencia during a period of 4 years, from January 2006 to December 2009. The criteria for inclusion in the study were the presence of hitherto undiagnosed alveolar infiltration, as evidenced by thoracic radiology, accompanied by a diagnostic profile consisting of a high temperature (>38°), coughing, expectoration, thoracic pain, dyspnea or tachypnea, and the absence of an alternative. The following patients were excluded from the study: patients who had already been admitted during the preceding 15 days; patients readmitted during the 30 days following their initial inclusion; HIV positive; patients who have undergone immunosuppressant and/or corticoid treatment (>10mg/day) during the preceding 6 months and patients with HCAP (Healthcare-associated pneumonia).4
Socio-demographic data, information concerning comorbidities, the length of time during which the clinical picture had been developing, vital signs and antibiotic treatments prescribed before the patients’ arrival in hospital and the admission procedures. A microbiological study was carried out on all patients, as well as a severity evaluation, based on the Fine PSI (pneumonia severity index)5 and CURB-65.6 For the microbiological diagnosis, the following procedures were applied: (a) S. pneumonia and the Legionella pneumophila serogroup 1 antigen detection in concentrated urine using the Binax Now® (Binax company); (b) detection of bacteria in pleural liquid, in the event of a significant pleural effusion, in the sputum and in fibrobronchoscopy samples by general culture methods such as chocolate agar and more selective ones such as MacConkey agar for the culture of gram negative bacteria, MSA (Mannitol Salt Agar) for Staphylococcus aureus and CNA (Columbia colistin-nalidixic acid agar) for gram positive cocci. Microbial identification and sensitivity tests were carried out using the VITEK® 2 (BioMérieux) system. In the case of the sputum samples, only those of good quality were analyzed (the presence of fewer than 10 epithelial cells and more than 25 leucocytes per field, with the 10× lens following Gram stain); (c) detection of bacteria in the blood by means of an automised BacT/Alert 3D® (BioMérieux) system. When bacterial growth was detected, a Gram stain and reculturing was carried out in the appropriate culture media. The microbial identification and the sensitivity tests were carried out using the VITEK® 2 (BioMérieux) system; (d) Serological methods were used, such as chemiluminescence for the detection of the L. pneumophila antigen in urine; ELISA for the detection of the L. pneumophila 1–7, M. pneumoniae, Varicella zoster virus antigens and respiratory viruses (Adenovirus, Parainfluenza virus 1, 2 and 3, Influenza virus A and B and Virus respiratorio Sincitial); and immunofluorescence for Coxiella burnetti and Chlamydophila pneumoniae. Serum was obtained for the detection of specific antibodies against Mycoplasma pneumoniae, C. burnetti, C. pneumoniae, L. pneumophila and respiratory viruses (Adenovirus, Parainfluenza virus 1, 2 and 3, Influenza virus A and B y Virus respiratorio Sincitial) in 2 samples separated by a period of 21 days. Positive antigens for pneumococcus or Legionella, positive culture in pleural liquid, positive sputum cultures in the case of primary pathogens, quantitative positive cultures in samples obtained by means of bronchoscopy (with bacteria counts exceeding 103UFC/ml in the case of protected brushing and greater than 104UFC/ml in the case of bronchoalveolar lavage), positive results in 2 consecutive hemocultures, were regarded as diagnostically significant etiological criteria on the NAC1 test. In the serological study, diagnostic significance was attributed to the detection of specific type IgM antibodies and/or at least a 4-fold increase in the specific type IgG antibody titers (seroconversion) between the 2 samples of serum obtained during a period of 3 weeks (the first sample being collected during the acute phase of the illness and the second during convalescence).
Subsequently, the study was completed with a clinical/radiological evaluation accompanied by a fresh collection of blood samples after 21 days of the development of the condition with a view to studying the serological conversion to different atypical germs responsible for CAP, and mortality data were collected during hospitalisation and 30 days after diagnosis.
The seasons of the year were defined as spring (March, April and May), summer (June, July and August), autumn (September, October and November) and winter (December, January and February), in accordance with the criteria established by the National Institute of Meteorology and the Environment.7 The meteorological data used to evaluate climatological change during the 4 consecutive years of the study included the average seasonal temperature and average accumulated rainfall for each of the different seasons of the year. The source employed for the average seasonal temperature and average accumulated seasonal rainfall during the course of the 48 months of the study was the Fundación Centro de Estudios Ambientales del Mediterráneo Programa de Meteorología-Climatología.8
Statistical AnalysisThe data were tabulated and analyzed in a database designed for the purpose within the statistical programme SPPS for Windows, version 12.0 (2003 SPPS Inc, Chicago, Illinois, USA). A statistical analysis was carried out of the qualitative and quantitative variables for the purpose of classifying the study population. The frequency distribution was analyzed and the central tendency measures, the standard deviation and confidence intervals were calculated at 95%. The comparison and proportions between groups was carried out using the Chi squared test, with the Fisher exact formula being applied when necessary. The comparison between quantitative variables was carried out by means of the Student's t-test for independent samples and variance analysis, according to variance normality and homogeneity assumptions. The Pearson or Spearman correlation was used to observe the association between variables. A value of P>.05, two-tailed, was considered significant.
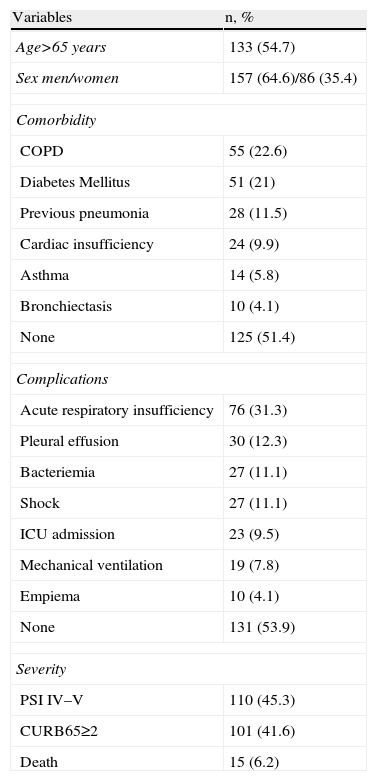
ResultsDuring the study period a total 243 patients were included, with an average age of 63.92±17.04, 157 (64.6%) of whom were male and 86 (35.4%) female. Table 1 shows the main demographic characteristics, comorbidity, severity and complications in patients.
Demographic Variables, Comorbidity, Complications (n=243).
| Variables | n, % |
| Age>65 years | 133 (54.7) |
| Sex men/women | 157 (64.6)/86 (35.4) |
| Comorbidity | |
| COPD | 55 (22.6) |
| Diabetes Mellitus | 51 (21) |
| Previous pneumonia | 28 (11.5) |
| Cardiac insufficiency | 24 (9.9) |
| Asthma | 14 (5.8) |
| Bronchiectasis | 10 (4.1) |
| None | 125 (51.4) |
| Complications | |
| Acute respiratory insufficiency | 76 (31.3) |
| Pleural effusion | 30 (12.3) |
| Bacteriemia | 27 (11.1) |
| Shock | 27 (11.1) |
| ICU admission | 23 (9.5) |
| Mechanical ventilation | 19 (7.8) |
| Empiema | 10 (4.1) |
| None | 131 (53.9) |
| Severity | |
| PSI IV–V | 110 (45.3) |
| CURB65≥2 | 101 (41.6) |
| Death | 15 (6.2) |
COPD, chronic obstructive pulmonary disease; ICU, Intensive Care Unit; PSI, pneumonia severity index; CURB65, confusion, urea, respiratory rate, blood pressure, over 65 years.
Among the pathological antecedents it is worth highlighting in particular the fact that 22.6% of the patients were diagnosed with COPD and 21% with diabetes Mellitus. 45.3% were classified as PSI IV–V and 41.6% as CURB65≥2 at the time of diagnosis. The most frequent complication was acute respiratory insufficiency, in 31.3% of patients. 9.5% of the patients required admission to the ICU and 15 patients died (6.2%) during the episode.
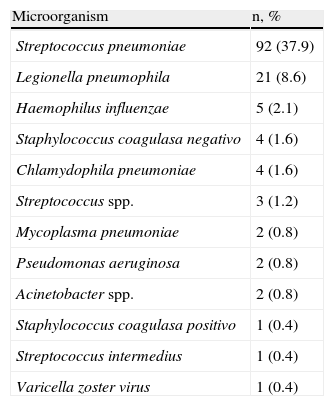
Table 2 shows the different isolated microbiological agents responsible for the conditions. In 139 cases (57.2%) we obtained a reliable etiological diagnosis. The most common isolated micro-organism was Streptococcus pneumoniae in 92 patients (37.9%) followed by L. pneumophila, responsible for 21 NACs (8.6%).
Etiological Microorganism.
| Microorganism | n, % |
| Streptococcus pneumoniae | 92 (37.9) |
| Legionella pneumophila | 21 (8.6) |
| Haemophilus influenzae | 5 (2.1) |
| Staphylococcus coagulasa negativo | 4 (1.6) |
| Chlamydophila pneumoniae | 4 (1.6) |
| Streptococcus spp. | 3 (1.2) |
| Mycoplasma pneumoniae | 2 (0.8) |
| Pseudomonas aeruginosa | 2 (0.8) |
| Acinetobacter spp. | 2 (0.8) |
| Staphylococcus coagulasa positivo | 1 (0.4) |
| Streptococcus intermedius | 1 (0.4) |
| Varicella zoster virus | 1 (0.4) |
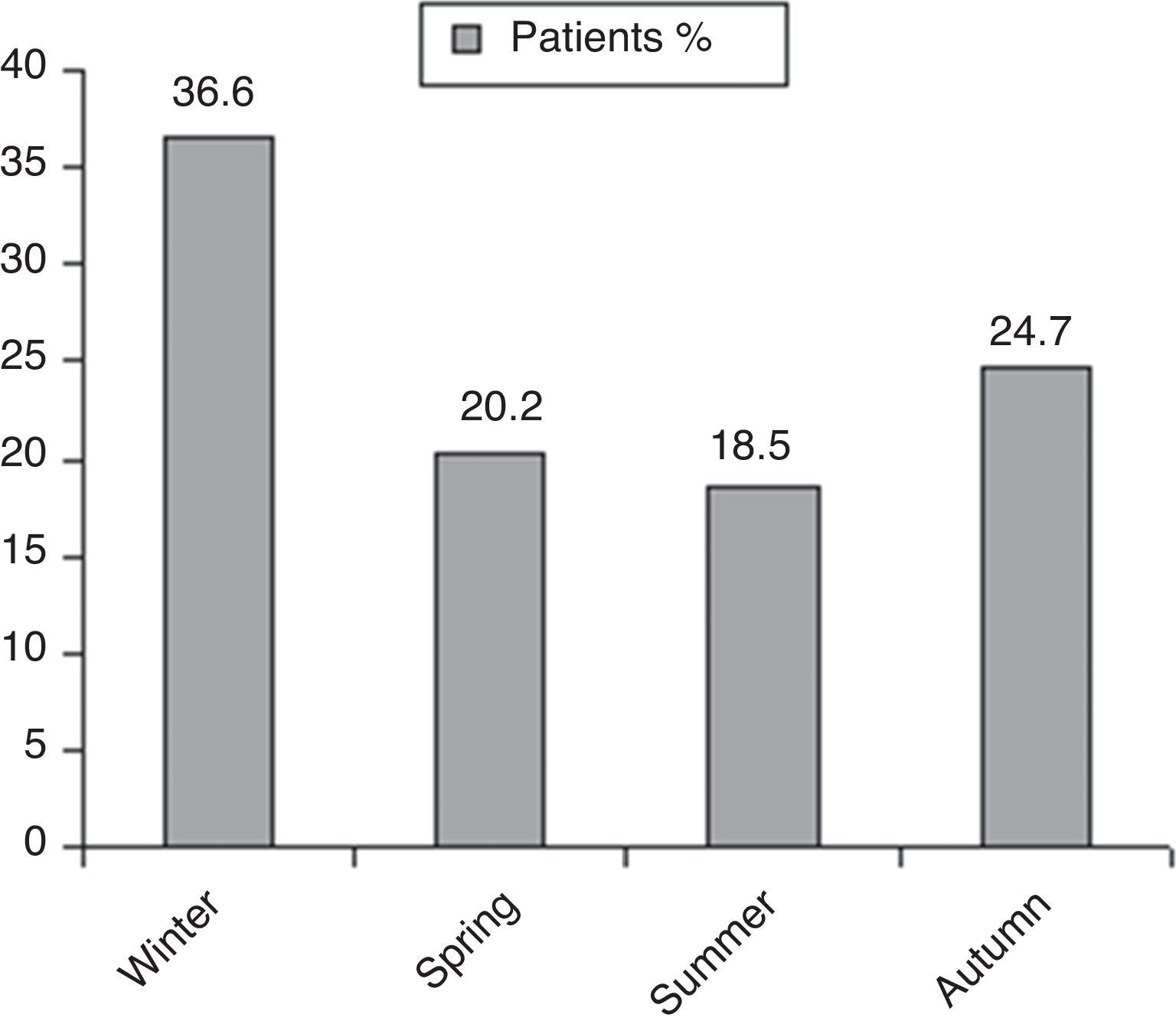
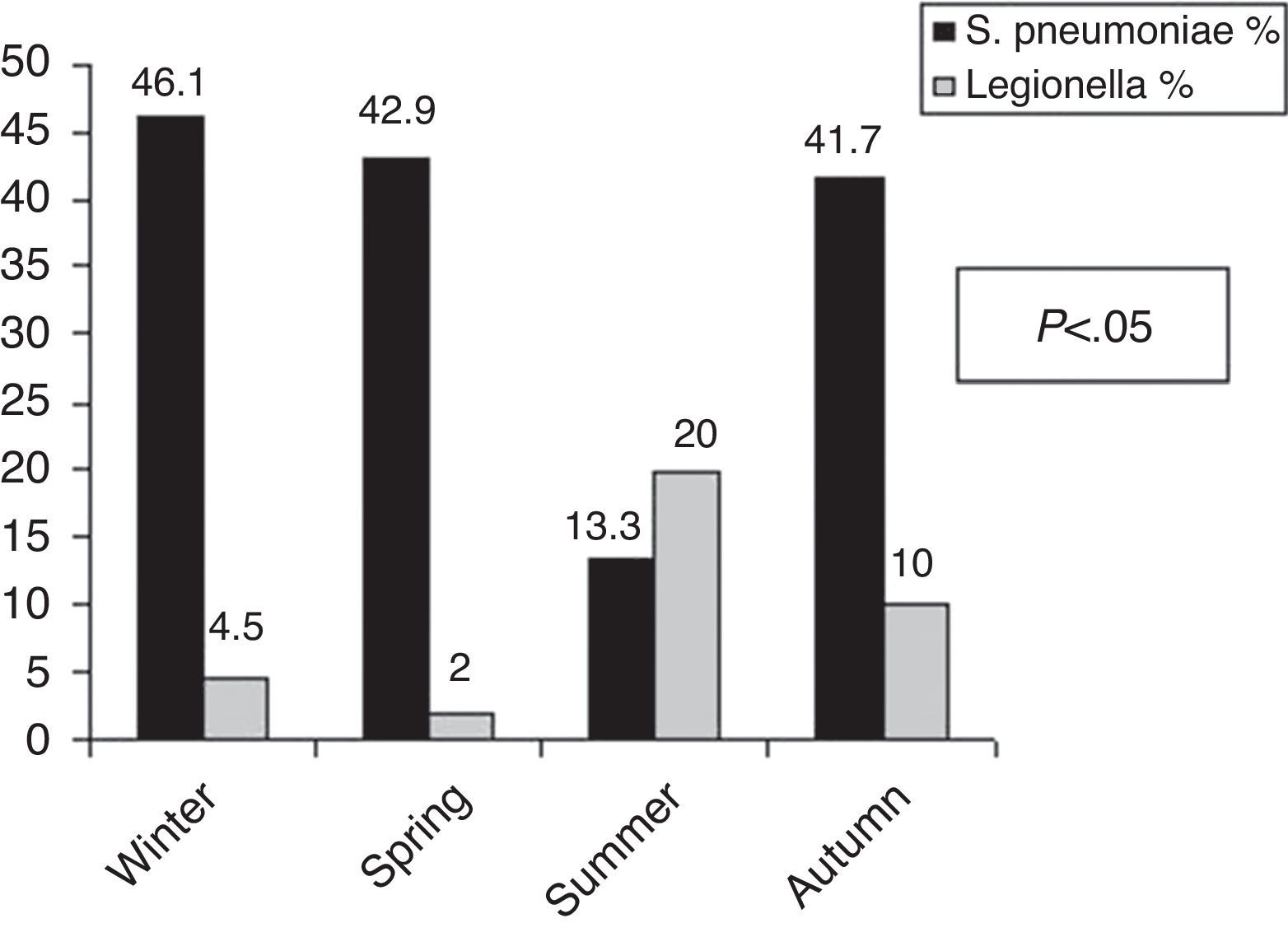
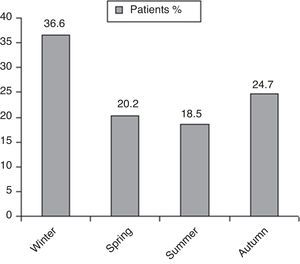
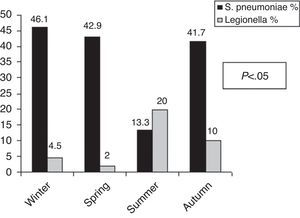
Seasonal distribution analysis showed a greater incidence of CAP in winter (Fig. 1). Statistically significant differences were found with regard to the micro-organism responsible in relation to the season of the year (Fig. 2). Thus 46.1% of the CAP admitted in winter, 42.9% of those admitted in spring and 41.7% of those admitted in autumn were caused by S. pneumoniae, while 20% of the CAP admitted in the summer were caused by L. pneumophila (P<.05).
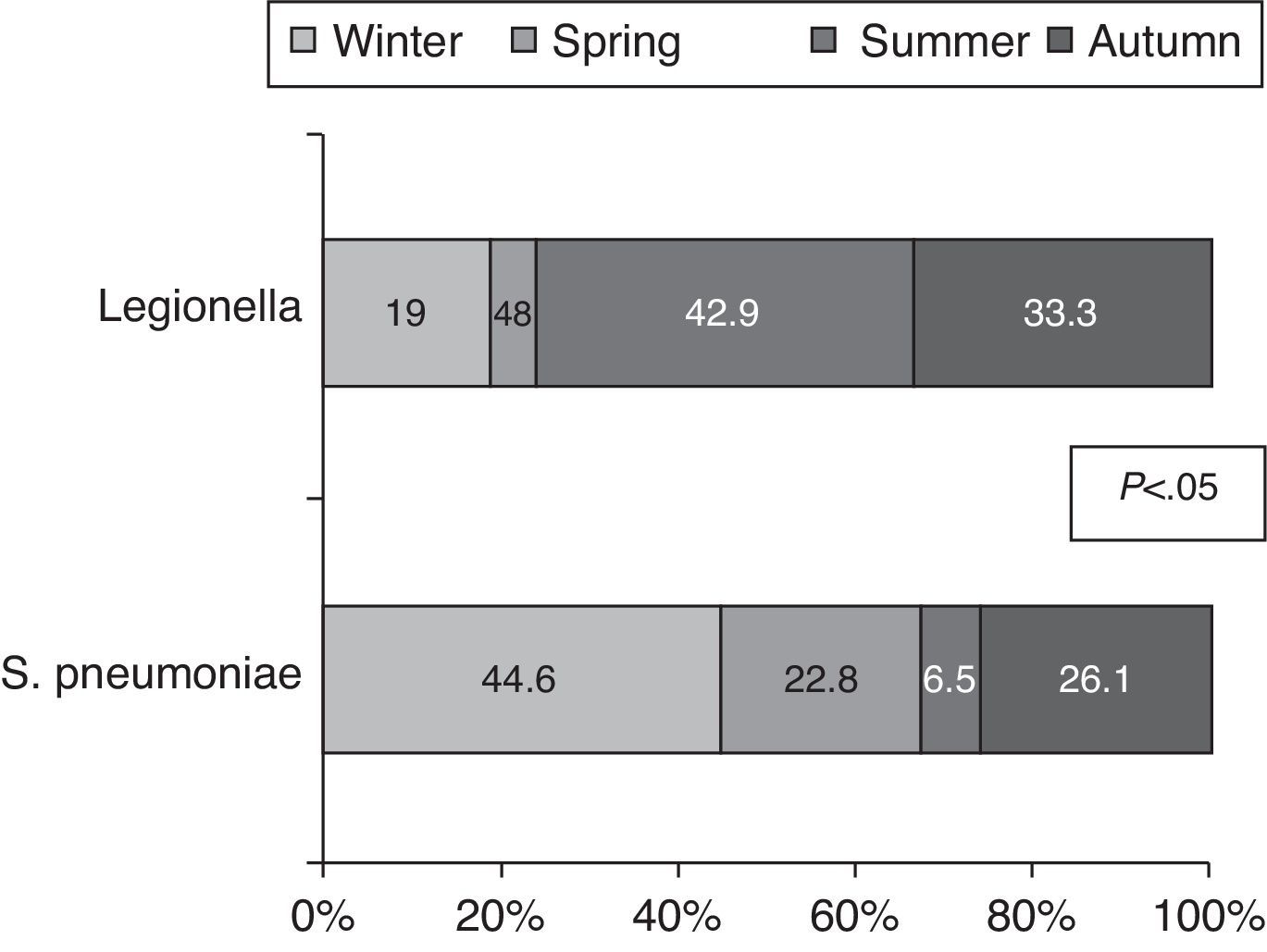
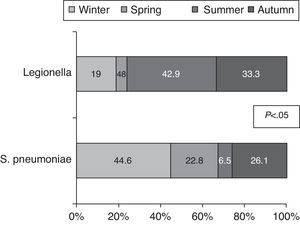
Similarly, the incidence of S. pneumoniae and L. pneumophila varies depending on the season; thus, 44.6% of the cases of S. pneumoniae occur in winter and 42.9% of Legionella in summer (P<.05) (Fig. 3).
No differences were found between the different demographic variables, comorbidity, complications, severity as evaluated by prognosis scales, or the number of deaths in relation to the season.
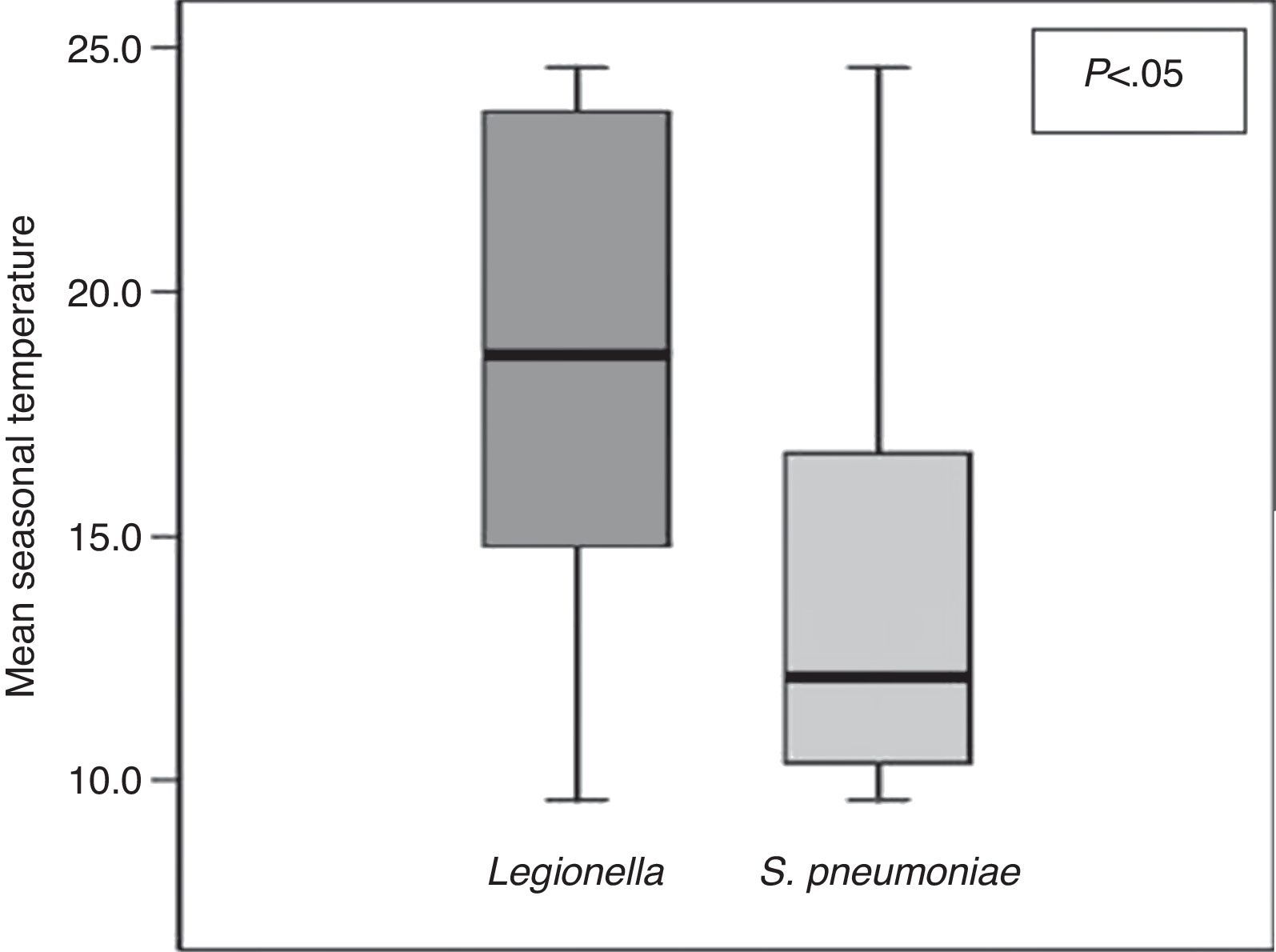
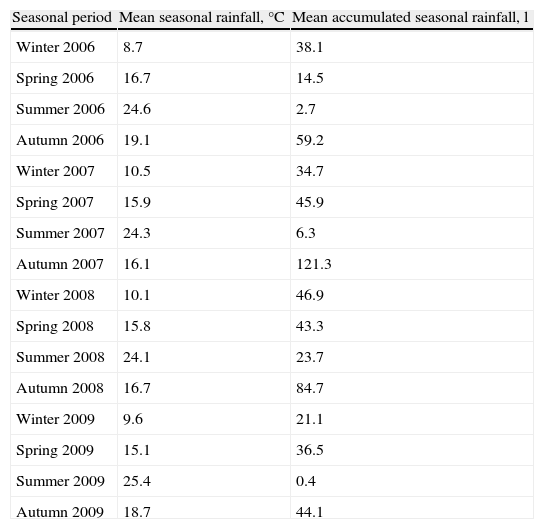
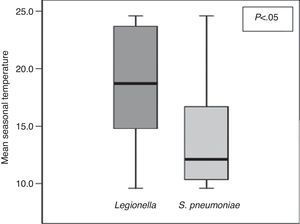
To analyze the influence of the climatological data concerning average seasonal temperature in each season of the year and average seasonal rainfall during the period of the study (Table 3). We observed a significant influence of average seasonal temperature on the causal micro-organism, so that S. pneumoniae predominated at lower temperatures than Legionella pneumophila (Fig. 4). Furthermore, we observed a significant correlation between the lowest average seasonal temperature and the CAP pneumococcal etiology (r=−0.33, P<.05), and the other way round with regard to the CAP for L. pneumophila (r=0.24, P<.05). As regards atmospheric humidity, as defined by the average accumulated rainfall, no significant differences were found.
Mean Seasonal Temperature, Mean Accumulated Seasonal Rainfall and Quantity of Rainfall per Season of the Year.
| Seasonal period | Mean seasonal rainfall, °C | Mean accumulated seasonal rainfall, l |
| Winter 2006 | 8.7 | 38.1 |
| Spring 2006 | 16.7 | 14.5 |
| Summer 2006 | 24.6 | 2.7 |
| Autumn 2006 | 19.1 | 59.2 |
| Winter 2007 | 10.5 | 34.7 |
| Spring 2007 | 15.9 | 45.9 |
| Summer 2007 | 24.3 | 6.3 |
| Autumn 2007 | 16.1 | 121.3 |
| Winter 2008 | 10.1 | 46.9 |
| Spring 2008 | 15.8 | 43.3 |
| Summer 2008 | 24.1 | 23.7 |
| Autumn 2008 | 16.7 | 84.7 |
| Winter 2009 | 9.6 | 21.1 |
| Spring 2009 | 15.1 | 36.5 |
| Summer 2009 | 25.4 | 0.4 |
| Autumn 2009 | 18.7 | 44.1 |
The most important findings of our study are: (1) that the season of the year when most cases of CAP were admitted was winter; (2) S. pneumoniae was the most common causal micro-organism in seasons of the year other than summer, when it was L. pneumophila; (3) most isolated cases of S. pneumoniae in our series appear in winter and L. pneumophila in summer; (4) we observed an influence of the mean seasonal temperature and the causal micro-organism, with a significant correlation between the the lowest mean seasonal temperature and the CAP pneumococcal etiology while the opposite was the case for the CAP for L. pneumophila; and (5) no relationship was found between the seasonal atmospheric humidity variations and the CAP etiological differences.
CAP is a common disease which is a significant cause of morbidity and mortality throughout the world, and a frequent reason for admission to hospital. The incidence of the condition in Spain is estimated to be 219 per 100000 inhabitants per year.9,10
The seasonal aspect of the illness has to do with the fact that its incidence increases systematically during a particular season of the year. In order that hospital services be planned more effectively and the pathogenesis of the disease be better understood, it is necessary to know, not only what the epidemiological variables are, but also whether or not it is associated with seasonal variation and, if this is the case, what its distribution is and what climatological variables it depends on. However, despite the high incidence of CAP and the seasonal variations that can be observed, this factor has been the subject of very little analysis in the relevant literature. For the most part, research has focused on seasonal variations in morbidity and mortality associated with V. influenza.3 On the other hand, the incidence of CAP is difficult to establish due to the variability and design of the studies, the target populations and the geographical location. Even so, independent of these variables, the consensus is that the incidence is higher during the winter months.11 On the basis of the findings of our study, we can affirm that in our geographical area, the largest number of hospital admissions due to CAP occurs in winter. These results are similar to those of other studies carried out in Spain,2 Israel12 and Taiwan.13
As regards etiology, the most frequent causal micro-organism for CAP is S. pneumoniae,14,15 although variability has been documented in relation to geographical area.16 In our series, the incidence of S. pneumoniae, as has been observed in previous studies,17–19 is greater in winter whereas in summer cases of L. pneumophila are more prevalent. The latter are all sporadic, although in our area outbreaks associated primarily with the summer have been observed.20 Similarly, other authors in the USA,21 Canada,22 ad Scotland,23 describe a greater incidence of L. pneumophila both in summer and autumn. These results differ from those of other studies carried out in Israel12 and Spain,24 where no seasonal predominance was observed.
Most published studies have focused their seasonal research of CAP predominance depending on the season of the year both on the etiological micro-organisms and on age and sex differences. In relation to the latter, there are studies which have documented the fact that aging is associated with a greater risk of CAP due to S. pneumoniae and the flu virus.25 On the other hand, Lieberman et al.26 observed a greater number of hospital admissions due to CAP in winter in individuals under the age of 16, while other studies, such as those conducted by Lin et al.13 and Säynäjäkangas et al.3 reflect a similar pattern across the age groups. Neither of the 2 studies,3,13 observes any seasonal variation in relation to the sex of the patients. These results coincide with ours, as we likewise noticed no seasonal differences in the age or sex variables.
Besides the well-documented seasonal variability in infectious diseases, temperature and humidity, as climatological variables, are significant determining factors in the survival of the pathogens. The low temperatures and a diminution of atmospheric humidity are associated with a greater incidence of the respiratory tract.27 On the other hand, the greater incidence of invasive pneumococcal illness during periods of a decrease in ultraviolet radiation, can be explained by their direct effects on the survival of the germ or alteration of the immune function in the metabolism of 1.25-(OH)2-vitamin D.28 In this way, meteorological factors are relevant to the incidence of the disease; on the other hand, other studies carried out in regions such as Israel and Taiwan show results which cannot easily be extrapolated to other geographical areas like ours, with different temperature and humidity ranges. In this sense, Lin et al. found that each degree by which the temperature falls is associated with an increase in the monthly admission for pneumonia of 0.03/10000 inhabitants. In our series, it was possible to show causal micro-organism variation (S. pneumoniae and L. pneumophila) in relation to seasonal change, and also to evaluate the influence of climate change within the different seasons of the year, on the basis of the observation that the mean seasonal temperature impacts significantly on the etiology of CAP. In our geographical area, low temperatures correlate with a greater incidence of pneumococcal pneumonia and high temperatures with those caused by L. pneumophila. However, we did not find atmospheric humidity to influence CAP etiology. This result contrasts with the study Fisman et al.,29 in which an association is described between humidity and the number of cases of Legionella, perhaps because our study only contains data concerning patients hospitalised for CAP, and excludes less severe cases.
One important aspect of our study, by contrast with others, is that it is not limited to one single year; we believe that it would be unreasonable to confine this seasonal variation to this single period of time, as the findings concerned can be causal and not due to a phenomenon that is effectively repeated annually. Nevertheless, we must consider the possibility that our results, which show clear seasonal etiological distribution, could be an epidemic lasting several years, with seasonal outbreaks during certain periods of the year throughout each of the years of the hypothetical epidemic.
Another aspect which warrants some consideration is the analysis that has been carried out on the influence of the meteorological factors relating to our geographical area, which could be extrapolated to other regions with similar temperature and humidity ranges.
The main limitation of the study is that only data concerning patients admitted to the Pulmonology Unit were obtained, and patients admitted to other units were excluded, such as Internal Medicine (Geriatric Unit), where elderly patients tend to be admitted, and Short Stay Hospitalisation, with less severe cases of CAP.
Despite these limitations, our results show that the seasonal distribution of CAP admissions is greater in winter, as is reflected in the literature11; that in our context, S. pneumoniae is the etiological agent that predominates in winter and L. pneumophila is the one that prevailed in the summer, in clear association with the fall in mean seasonal temperatures for pneumococcal, while the reverse was the case for Legionella.In our context, the availability of such results is relevant, as the few studies that have researched the relationship between these climatological and seasonal parameters and hospitalised cases of CAP, refer to other geographical areas, and are therefore, difficult to extrapolate to ours, with different temperature and humidity ranges.
Conflict of InterestThe authors have no conflict of interest to declare.
Please cite this article: Herrera-Lara S, et al. ¿Influyen la estación y el clima en la etiología de la neumonía adquirida en la comunidad? Arch Bronconeumol. 2013;49:140–5.