Hydatid disease (also known as hydatidosis or echinococcosis) is a worldwide zoonosis produced by the larval stage of the Echinococcus tapeworm. In humans, the liver is the most commonly affected organ (70% of cases approximately), followed by the lungs (25%); from these anatomical locations, the disease locally involve neighbor organs or extend to distant sites.
The accepted treatment includes surgery, when feasible, and systemic anthelmintic drugs. Despite this treatment, a significant percentage of patients unfortunately present an early or late recurrence of the disease (in surgically treated cases ranges from 0 to 22%1).
We present the case of a 69 year-old male who was referred to our department with a painless non-inflammatory mass involving the right posteroinferior chest wall and the paravertebral muscles. His past medical history included a right nephrectomy, performed fifty years earlier for renal hydatidosis.
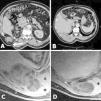
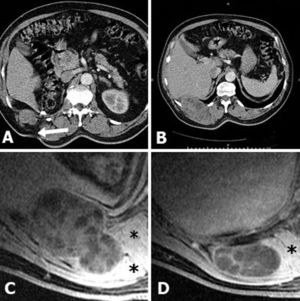
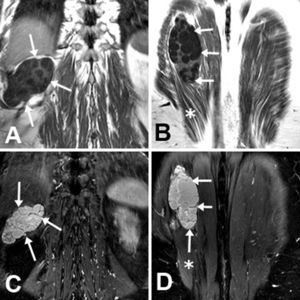
A whole-body computed tomography (CT) revealed a large multilocular cystic mass originating at the remote lumbotomy scar and invading ipsilateral posteroinferior chest wall, diaphragm, and right paravertebral muscles (Fig. 1A, B). A Magnetic Resonance imaging (MRI), performed to better define the lesion, confirmed the CT findings (Figs. 1C, 1D and 2).
(A, B) CT. Multicystic mass which originates from the lumbotomy scar (arrow). (C, D) Axial fat-suppressed gadolinium-enhanced T1-weighted MRI. Multilocular cystic mass (arrows) extending from the right nephrectomy bed into the posteroinferior thoracic wall and paravertebral muscles (asterisks). Note the hourglass morphology in C.
With the clinical and radiological suspicion of relapsed hydatid disease, the patient was started with albendazole (10mg/kg/daily) for 15 days before surgical treatment.
In the operation room, we first resected the lumbotomy scar. After confirming the involvement of the right 11th intercostal muscle and the longissimus dorsi muscle, we decided to resect the last two right ribs along with the affected intercostal space, part of the right hemidiaphragm, and the right paravertebral muscles. Even though the multicystic mass abutted the pleural space, the pleural cavity remained unaffected. Gauzes and cotton pads impregnated with hypertonic saline protected the surgical field. A PTFE (expanded polytetrafluoroethylene) patch was used to reconstruct the chest wall, to which the diaphragm was reattached. The patient was treated with mebendazole for six more months.
The final pathology report confirmed the suspected diagnosis of recurrent hydatid disease. After 26 months of follow-up, the patient continues asymptomatic and without signs of recurrence on imaging studies.
Hydatidosis is a significant public health problem in many countries around the world.
Its incidence in endemic areas ranges from 1 to 220 cases per 100,000 inhabitants, while the incidence of alveolar echinoccocosis ranges from 0.03 to 1.2 cases per 100,000 inhabitants, making it a much rarer form of echinococcosis.2
Spain is considered an endemic area for echinococcosis.3 The autonomous communities of Spain most affected by the disease are Aragón, Castilla La Mancha, Castilla y León, Comunidad Valenciana, Extremadura, and La Rioja, characterized by a high concentration of sheep and cattle farms.4
Since 1982 echinococcosis is a notifiable disease in Spain. With the gathered information by the different regional authorities, a public report is periodically published in the webpage of the Institute of Health Carlos III. According to the last report,5 the incidence in the most affected communities lies between 0.34 and 1.13 cases per 10,000 citizens.5
In humans, the most involved organs of hydatid disease are the liver (70%) and the lungs (25%). However, secondary involvement may be seen in almost any anatomic location.6 Involvement of skeletal muscle is much rarer for two reasons: first of all, to reach the muscles, the parasite must cross both the hepatic and the pulmonary barriers; and secondly, the presence of lactic acid in the muscles creates a hostile environment for the development of the cyst.6,7
The diagnostic imaging tests ultrasound (US) and CT are useful for diagnosing the disease, for suggesting viability of the cysts, and for describing the internal features of the lesion, its location, and the involvement of adjacent organs. The characteristic lesion is usually seen as a well-defined spherical- or oval-shaped, uni- or multilocular cyst, with varying wall thickness. MRI is the diagnostic method of choice for evaluating hydatid disease involving the soft tissues and is also useful for planning the surgical approach.
There is a general agreement that the most effective treatment is radical surgery with a complete excision with intact cyst wall.8 Medical therapy is a complementary treatment to reduce the risk of early relapse. Even though percutaneous fine needle aspiration may help in the preoperative management of large cysts or as a non-surgical treatment in inoperable cases, however, it could carry a higher risk of in-field dissemination. In addition, Voros et al.9 have reported the existence of small satellite cysts surrounding the pericyst wall; this may explain the high relapse rate seen in incomplete surgeries, in which there is a significant possibility of leaving viable parasites.
In conclusion, our patient presents a rare case of very delayed hydatid cyst relapse involving the paravertebral muscle fifty years after a nephrectomy performed for isolated renal hydatidosis. This case highlights the importance of being aware of this infectious disease, especially in endemic areas, taking into consideration the multiples faces with which this condition may manifest (including mimicking a soft tissue tumor). For this reason, it reminds us the importance of considering hydatid disease in the differential diagnosis of soft-tissue cystic tumors. Likewise, it illustrates the possibility of a delayed relapse of a previously resected hydatid cyst. In our case, the nephrectomy was performed fifty years earlier in another hospital, so it was not possible to investigate whether there was a rupture of the cyst during the procedure. Even though the optimal follow-up of patients with hydatid cysts has not yet been established, it should be at least of 3–5 years duration.8
We also want to underline the behavior of the parasite which, following the previous flank incision scar as a path, infiltrated the paravertebral space. To our knowledge this is the first case in which hydatid cyst disseminates locally following the incision scar without surgical bed recurrence.
Regarding our surgical approach, we decided to resect the cyst en-bloc, instead of performing a cysto pericystectomy, in order to avoid an accidental rupture of this large mass.
Radical en-bloc surgery, perioperative medical treatment, and chemical protection of the surgical field are necessary measures to successfully accomplish the goal of the treatment.