Pneumonia remains a leading cause of preventable illness and death in children under five years of age worldwide.1 Globally, pneumonia is associated with between 812,000 and 1.1 million deaths in children annually. In 2017 in Brazil, 2,551,218 hospital admissions occurred among children under five years old and regarding mortality, 3120 deaths due to respiratory disease were registered in the same age range.2
To add to this situation, in 2019 the first cases of COVID-19 were identified. Since then, the number of moderate to severe cases of COVID-19 has increased exponentially in hospitals worldwide, but the disease has consistently behaved benignly in most children compared to adults.3
The World Health Organization and the Centers for Disease Control recommended COVID-19 policies implementation as part of the preemptive and contention measures for COVID-19.4 Since then, studies have shown that, in 2020, there was a reduction in general pediatric care, emergency department visits, and hospital admissions of infants with bronchiolitis.5,6 The aim of this study is to analyze the impact of those initiatives, originally against COVID-19, on hospitalization mortality due to community-acquired pneumonia in Brazilian children.
This ecological study analyzed the data on hospital admissions and deaths due to community-acquired pneumonia in children and adolescents occurring in Brazil from 2019 to 2020. The data were obtained from the database of the Department of Informatics of the Brazilian Public Health System (DATASUS).6,7
Poisson regression models with robust variance were used to obtain relative risk (incidence of hospitalizations or mortality pre-PCPI/incidence of hospitalizations or mortality with PCPI in place) and the respective 95% CI. The cut-off probability for rejecting the null hypothesis was defined as less than 5%. The statistical analysis was performed using the R software (www.r-project.org/) and the statistical analysis was performed using the IBM SPSS Statistics for Windows, version 21.0.
This study does not contain personal or individual data, so it was considered exempt from evaluation by the Research Ethics Committee.
From 2019 to 2020, 328,307 hospital admissions and 2383 deaths due to pneumonia were identified in children and adolescents up to 19 years of age. The risk of hospitalization for pneumonia in children in the period when COVID-19 policies implementation measures were implemented to contain de pandemic (2020) was 68% lower compared to 2019 (RR=0.32; 95% CI: 0.29 to 0.37) and that of mortality from pneumonia during hospitalization was 50% lower (RR=0.50; 95% CI: 0.44 to 0.58). Children under the age of 12 months saw the greatest reduction in hospitalizations (RR=0.27; 95% CI: 0.23 to 0.31) and mortality (RR=0.49; 95% CI: 0.40 to 0.59) (Table 1).
Mean annual incidence, relative risk, and 95% confidence interval of hospitalizations and mortality due to pneumonia in Brazilian children by age range.
| Hospitalization | Mean incidence | RR | Lower 95% CI | Upper 95% CI | Mortality | Mean incidence | RR | Lower 95% CI | Upper 95% CI | |
|---|---|---|---|---|---|---|---|---|---|---|
| <12 months | ||||||||||
| 2020 | 58.8 | 0.27 | 0.23 | 0.31 | 0.88 | 0.49 | 0.40 | 0.59 | ||
| 2019 | 215.4 | 1 | 1.78 | 1 | ||||||
| 1–4 years | ||||||||||
| 2020 | 25.6 | 0.31 | 0.27 | 0.35 | 0.12 | 0.43 | 0.35 | 0.55 | ||
| 2019 | 82.4 | 1 | 0.28 | 1 | ||||||
| 5–9 years | ||||||||||
| 2020 | 7.29 | 0.39 | 0.35 | 0.44 | 0.03 | 0.38 | 0.28 | 0.52 | ||
| 2019 | 18.4 | 1 | 0.09 | 1 | ||||||
| 10–14 years | ||||||||||
| 2020 | 3.3 | 0.49 | 0.44 | 0.55 | 0.05 | 0.6 | 0.45 | 0.79 | ||
| 2019 | 6.6 | 1 | 0.08 | 1 | ||||||
| 15–19 years | ||||||||||
| 2020 | 2.7 | 0.55 | 0.49 | 0.62 | 0.09 | 0.65 | 0.53 | 0.79 | ||
| 2019 | 5.0 | 1 | 0.13 | 1 | ||||||
| Total | ||||||||||
| 2020 | 11.2 | 0.32 | 0.29 | 0.37 | 0.11 | 0.5 | 0.44 | 0.58 | ||
| 2019 | 34.1 | 1 | 0.22 | 1 | ||||||
RR: risk relative, CI: confidence interval.
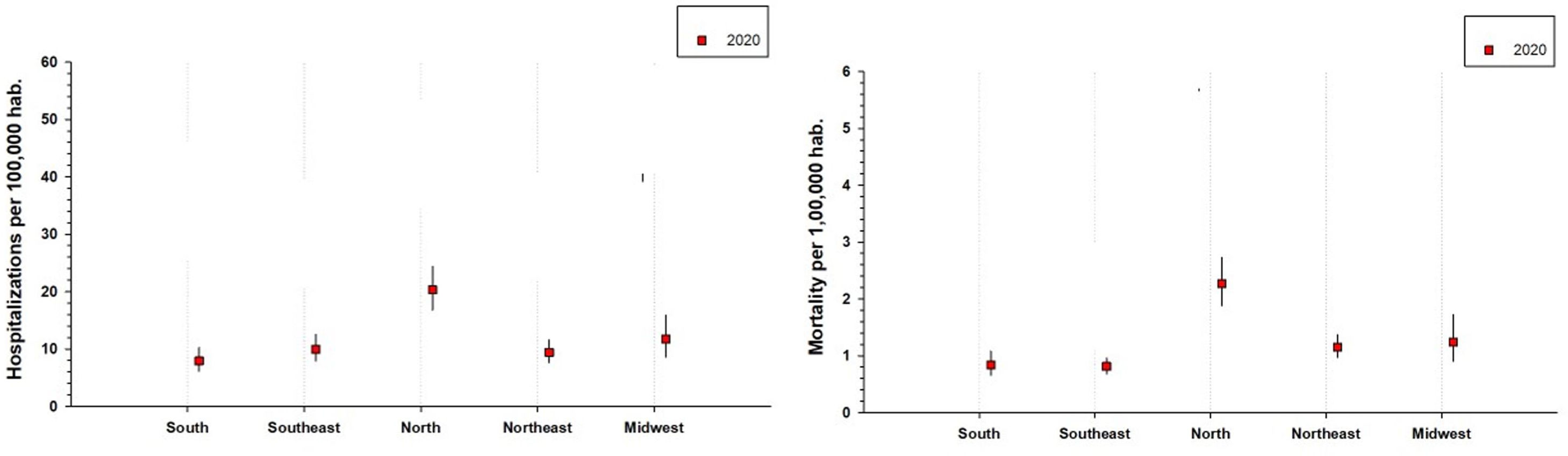
The same downward trend, albeit with different magnitudes, was observed in different regions of Brazil. The South region saw the greatest reduction in hospitalizations for pneumonia in all age groups (Table 1). For mortality, the South region saw the greatest reduction only for the <12 months and the 10–14 years old age groups. Regarding the other age groups, the greatest reduction in mortality in children aged one to four years old was found in the Southeast, for those aged five to nine it was in the Midwest, and for those aged 10–15 it was in the North. When comparing the total incidences between the regions of Brazil, the highest incidence of hospitalizations and mortality was found in the North region (Fig. 1).
The overall cost of hospitalizations for pneumonia in Brazil was 43,552,662.88 dollars in 2019 and 16,200,443.39 dollars in 2020. In other words, Brazil saw a 63% reduction in the cost of hospitalizations for pneumonia when the COVID-19 prevention policies were applied.
Our study suggests that the policies for COVID-19 prevention were associated with an important decrease in pediatric hospital mortality in Brazil due to community-acquired pneumonia.
We believe that the implementation of policies for supporting COVID-19 prevention was the main reason for this reduction in pediatric pneumonia admissions and mortality during the first year of the COVID-19 pandemic in Brazil. It is not possible or feasible to pinpoint the individual contribution of the different policies for supporting COVID-19 prevention, but studies of the dynamics of their implementation propose that it is the combination of them that has proven to be most useful.5
At the same time, there are reports of an overall decrease in acute respiratory illnesses in children, as well as fewer emergency department visits and fewer pediatric hospital and intensive-care admissions for ARI during the pandemic.5–8 We did not identify any other studies that reported a decrease in child mortality from pneumonia during hospitalization. A recent study also found a significant decrease in cases of all cause pneumonia in Brazilian children under 14 years during the COVID-19 pandemic.9
For the present study, we performed a nationwide level analysis, and the results showed the same decreasing trend. The Southern region was the one with the greatest overall reduction in the incidence of hospitalizations for pneumonia. For mortality, the Southern region had the greatest reduction only in the age group <12 months.
With the COVID-19 pandemic, the main Brazil public health responses have been organized at the state and municipality levels, resulting in different choices and timing regarding the implementation of COVID-19 prevention policies. Social inequality in Brazil is a problem that affects a large part of the population, and the COVID-19 pandemic threatens to increase it even more.
A national average adherence of social distancing was <25% was reported, while the WHO believes at least 50% compliance is needed to have a noticeable effect.8 However, we believe that this low adherence applies mainly to adults, since children were subject to greater social distancing while staying at home and out of schools/daycare.10
The promotion of COVID-19 prevention policies needs to be constant and consistent in order to the spreading of viruses in both clinical settings and the community.11 In practical terms, hand hygiene, better space ventilation and even mask wearing during acute respiratory infections, should be included in health education programs.12–14 These simple strategies are cost-effective and feasible to apply at the different settings, such as schools, public transportation, workplaces and healthcare environments.12–19 In fact, the overall spending on pneumonia hospitalizations in Brazil was 63% lower during the COVID-19 prevention policies implementation period (2020) compared to 2019.
Our study has some limitations. We retrospectively obtained the data from the Brazilian health department registry system. However, this is the official system used to collect and analyze data for public health measures, and it has been effectively in place for more than a decade. We also did not have access to viral identification, which could provide a better picture of the impact the COVID-19 pandemic had on specific respiratory viruses. Nonetheless, pneumonia hospitalizations and mortality showed an important and consistent reduction in all age groups in all Brazilian regions, which suggests that all viruses were similarly affected.
Our study found an important reduction in hospitalizations mortality due to pneumonia, as well as in the cost of hospitalizations due to respiratory diseases, because of the implementation of COVID-19 prevention policies initiatives in the public health system. This reinforces the usefulness of prevention policies for decrease pneumonia mortality.
Summary of the article's main pointOur study found an important reduction in hospitalizations mortality due to pneumonia, as well as in the cost of hospitalizations due to respiratory diseases, because of the implementation of COVID-19 prevention policies initiatives.
FundingThis research has not received specific aid from public sector agencies, commercial sector or non-profit entities.
Conflict of interestThe authors declare that they have no conflict of interest directly or indirectly related to the contents of the manuscript.
Fundação de Amparo à Pesquisa do Rio Grande do Sul (FAPERGS), the National Research Council of Brazil (CNPq) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior CAPES Finance Code 001.