More and more biologics are being used for the treatment of severe asthma and it is convenient to know the available data about their cost-effectiveness in our healthcare setting. The studies carried out in other countries cannot be extrapolated to the scope of the Spanish national health system (SNS), so their own studies are needed. In Spain it is common for medicines to have a public price (notified) and a confidential one for the SNS (financed) and this makes it difficult to draw absolutely reliable economic conclusions. Most of the cost-effectiveness or cost-utility studies use the notified price (they cannot be done otherwise because the real price is confidential) and this circumstance must be taken into account; In the same way, the prices of the drugs are not constant over time and the temporality in which the study has been carried out must be considered. The good news is that the financed price is usually lower than the one reported. Taking these circumstances into account, we are going to analyze the main cost-effectiveness studies of biological therapy in severe asthma carried out in Spain.
All of real life analysis of the treatment of severe asthma with omalizumab results in significant improvement in asthma control and quality of life but pharmacoeconomic results are different. Levy AN (2014)1 in 47 patient of single centre, confirms that adding omalizumab to treatment reduces the number of exacerbations and the incremental cost-effectiveness ratio (ICERs) were 463 euros for exacerbation avoided and 26,864 euros/QALY gained. Vennera MC (2016),2 in single-centre study of 86 patients, the ICERs were €1130.93 (95% CI 909.08–1392.86) per exacerbation avoided, and €4124.79 (95% CI 3281.69–5186.73) per 3-point increase in the Asthma Control Test score (ACT). However, in a observational retrospective multicenter study conducted in 12 pneumology services of Martinez-Moragon E (2019)3 which included 186 patients, the incremental cost-utilty ratio per qualy adjusted life years gained were of 50,239 euros. Taking into account direct and indirect costs, the incremental cost-effectiveness for each avoided exacerbation was € 1789.28 (95% CI: € 1019.13–3038.12) and € 4569.38 (95% CI: 3442.86–6075.05) per 3-point increase in the ACT score. It is possible that when omalizumab was the only biologic available on the market, the same economic offers were not made to hospital pharmacies that have arisen when competition has increased.
With the rest of the biologicals that have been on the market for less time, we have little data available. Padilla-Galo A (2021)4 publishes a cross-sectional multicentre study of 44 consecutive patients with refractory eosinophilic asthma who received treatment with benralizumab during at least 12 months. Patient follow-up was performed in specialized severe asthma units. The total annual cost per patient for the baseline and benralizumab treatment periods were €11,544 and €14,043, respectively, reflecting an increase in costs due to the price of the biological agent but a decrease in costs for the remaining parameters. The ICER was €602 per avoided exacerbation and €983.86 for every 3-point increase in the ACT score.
Two studies have been published with indirect comparisons between biologics:
- -
Gonzalez-Barcalá FJ (2021)5 analyze the cost-effectiveness of mepolizumab with standard of care versus other anti-IL-5 therapies approved for the treatment of severe eosinophilic asthma patients, within the SNS perspective. A Markov model with a 4-week cycle length was used to compare. The analysis was performed over a 5-year time horizon. The model indicates that mepolizumab is dominant (lower cost, higher benefit) compared to benralizumab and reslizumab. For benralizumab and reslizumab, respectively, treatment with mepolizumab had a point estimate of 0.076 and 0.075 additional QALYs, and savings of €3173.47 and €7772.95 per patient. This study was funded by GlaxoSmithKline.
- -
Mareque M (2023)6 assess the cost-effectiveness of benralizumab vs. mepolizumab and dupilumab for the treatment of patients with severe uncontrolled asthma from the SNS perspective. Exacerbations avoided, QALYs gained and costs in a 5-year period were estimated with a Markov model for a cohort of 1000 patients in which, based on published evidence. Benralizumab was more effective (52.21 QALYs) than mepolizumab (51.39 QALYs) and dupilumab (51.30 QALYs). Benralizumab avoided more exacerbations (2.87 exacerbations) compared to mepolizumab (4.70 exacerbations) and dupilumanb (5.11 exacerbations) for the 5-year horizon. Total costs/patient were €56,093.77 (benralizumab), €59,280.45 (mepolizumab) and €62,991.76 (dupilumab), resulting in benralizumab dominating (more QALYs with lower costs). This study was funded by Astra-Zeneca.
These indirect comparisons represent biased data from the literature and do not take into account many confounding factors, for example that for some drugs the number of doses in all years is not similar since they have shock doses (benralizumab and dupilumab) and that if the populations are not identical, comparative studies and estimates cannot be made.
Type 2 inflammatory disease can present with various coexisting clinical manifestations and the addition of a biologic for the treatment of severe asthma can help control more than one disease; this circumstance should be considered in cost-effectiveness and cost-utility studies.
On the other hand, with biological therapy we reduce the steroid load of patients and although it is difficult to quantify in economic terms, presumably we are reducing the adverse effects of systemic corticosteroids with an associated reduction in costs for the SNS.
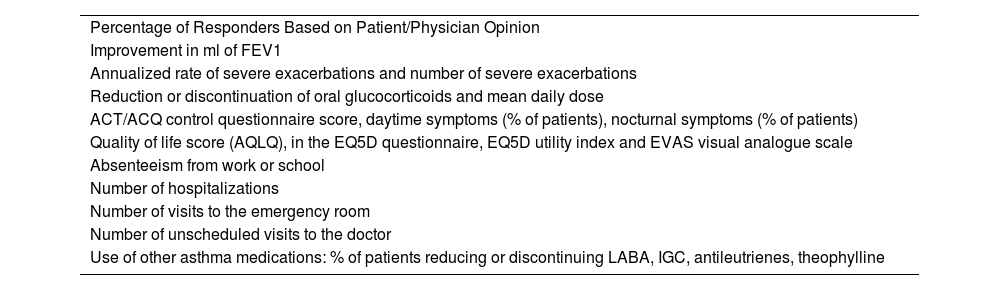
In summary, cost-effectiveness studies of biologics in asthma are very convenient but have major limitations in Spain, the biggest of which in our opinion is that the reported price is not the actual price of the drug. We do not have reliable comparative data between biologics. There is clear evidence that biologics improve quality of life, lung function, asthma control, and reduce exacerbations and the use of other asthma medications (Table 1) and that it is cost-efficient to prescribe them by experts and in asthma units,7 according to the guidelines of good clinical practice.8 The integrated treatment of patients with comorbidities associated with asthma using a biologic that can control them can be a saving tool for the SNS.
Variables of effectiveness used in real life studies with biologics in severe asthma.
| Percentage of Responders Based on Patient/Physician Opinion |
| Improvement in ml of FEV1 |
| Annualized rate of severe exacerbations and number of severe exacerbations |
| Reduction or discontinuation of oral glucocorticoids and mean daily dose |
| ACT/ACQ control questionnaire score, daytime symptoms (% of patients), nocturnal symptoms (% of patients) |
| Quality of life score (AQLQ), in the EQ5D questionnaire, EQ5D utility index and EVAS visual analogue scale |
| Absenteeism from work or school |
| Number of hospitalizations |
| Number of visits to the emergency room |
| Number of unscheduled visits to the doctor |
| Use of other asthma medications: % of patients reducing or discontinuing LABA, IGC, antileutrienes, theophylline |
The authors state that they have no conflict of interests.