Rounded atelectasis is a form of chronic lung collapse. The 2 main theories surrounding the origin of rounded atelectasis are the “collapse” theory (atelectasis due to pleural effusion) and the “fibrosis” theory (atelectasis due to pleural injury), both of which produce a rounded image on radiology.1 This radiological entity was first described in 1928, and since then it has been given a multitude of names, including “trapped lung”, “Blesovsky syndrome”, and “pseudotumor”.2 Pathogenesis can include exposure to mineral dusts (asbestos, silica, mixed mineral dusts), exudative pleural effusions (parapneumonic pleural effusion, tuberculosis effusion, hemothorax, post-cardiac surgery, chronic hemodialysis), or extrapulmonary causes (Legionella pneumonia, histoplasmosis, sarcoidosis, advanced renal impairment), pneumothorax, idiopathic injury, and, albeit more rarely, cancer. Rounded atelectasis is often revealed by a chance finding on an imaging test in an asymptomatic patient, and is generally visualized in standard X-rays as a rounded or oval subpleural opacity. It is usually solitary, and most commonly found in the upper lobes, although it also occasionally occurs in the middle lobe, lingula, or upper lobes. The image on standard radiography very often mimics that of malignant lesions, so other imaging tests are required. Rounded atelectasis appears on computed tomography (CT) as a subpleural nodule or mass. A characteristic sign of this radiological entity is the “comet tail sign”. These lesions are usually enhanced after administration of contrast medium, but this characteristic is indistinguishable from malignant neoplastic processes.
We report the case of a 67-year-old man with no known allergies, active smoker of 20 cigarettes/day, with moderate alcohol consumption. Personal history includes a psychotic disorder for which he is institutionalized. He receives regular treatment with risperidone and biperiden. Surgical history includes lumbotomy for urolithiasis and prostatectomy. In June 2015, he was diagnosed with a bladder tumor (pTa BG [II/III]) treated by transurethral resection. In October 2015, a chest CT was performed that revealed a peripheral pulmonary nodule in the right lung base in extensive contact with the pleura, measuring 2.7×1.7cm (Fig. 1A and B). In March 2016, a follow-up chest CT was performed, showing no clear changes in the lesion. Fine needle aspiration and biopsy was requested.
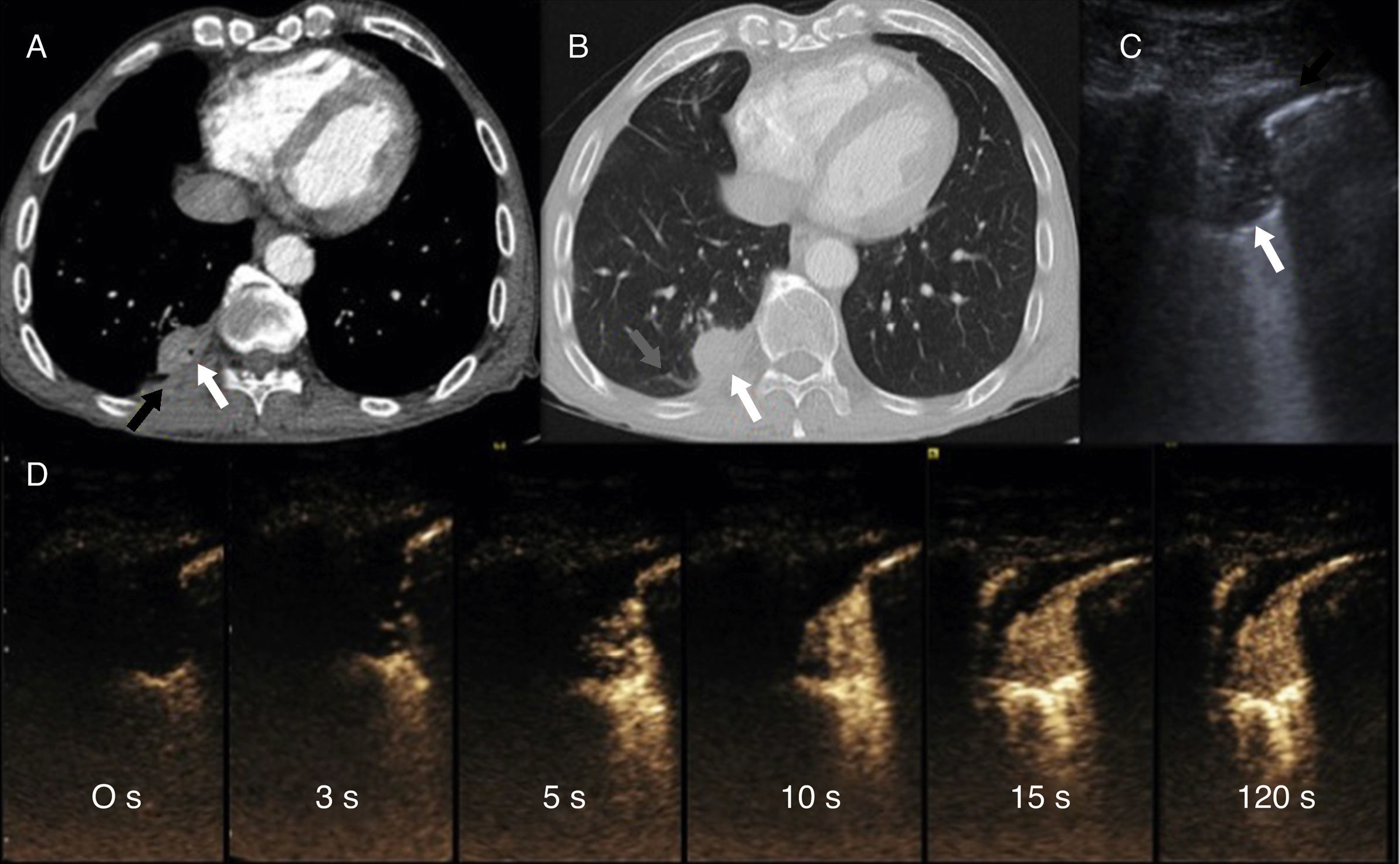
(A and B) Chest CT after intravenous administration of iodinated contrast medium, in the mediastinal window (A) and lung (B), showing a subpleural solid nodule (white arrow) with adjacent pleural thickening (black arrow) and bronchovascular incurvation (gray arrow). (C) Chest B-mode ultrasound: rounded consolidation (white arrow) associated with focal pleural thickening (black arrow). (D) Series of contrast-enhanced ultrasound images (time since administration of contrast appears in each image), demonstrating rapid uptake, earlier than 6seconds, that immediately becomes homogeneous and is not eliminated after more than a minute.
Although the radiological findings suggested rounded atelectasis, the suspicion of some lesion growth in the latest follow-up led us to rule out a malignant etiology. In this setting, we decided to perform ultrasonography with SonoVue® intravenous contrast (Bracco, Amsterdam, Netherlands) (Fig. 1C and D), with image-guided biopsy. Early (in the first 6seconds following administration), homogeneous uptake of the intravenous contrast medium by the tumor was observed on ultrasound. This uptake was maintained over time, and continued to be visible more than 1minute after the administration of contrast medium. These findings are highly suggestive of atelectasis. The biopsy results showed no atypia or other findings suggestive of a neoproliferative process.
The indications of contrast-enhanced ultrasound have increased in recent years,3 and several publications have described its usefulness in respiratory diseases.4–7 The lung is vascularized by 2 arterial systems, the pulmonary and the bronchial, and different diseases can be distinguished depending on the type of uptake. Lung cancers are generally irrigated by the bronchial arteries, so contrast uptake will be slower (longer than 7seconds) and may be heterogeneous, due to the presence of immature neovessels or necrosis. In contrast, atelectases are vascularized by the pulmonary artery, so uptake occurs earlier. Furthermore, contrast medium is typically not eliminated from atelectasis, but instead persists for some time (more than 1minute).8
Rounded atelectasis is a benign process that does not require treatment and generally resolves spontaneously or remains stable. Radiological monitoring is necessary to confirm its status. Nevertheless, on multiple occasions and in certain clinical contexts, histological (biopsy) or cytological (fine needle aspiration) specimens must be obtained to safely rule out underlying malignancy. Since atelectasis is usually located in a subpleural site, it can be easily visualized with ultrasound. Moreover, contrast-enhanced ultrasound is useful for characterizing these lesions. Accordingly, if we find a subpleural lesion with characteristics typical of atelectasis on a contrast-enhanced ultrasound, no invasive diagnostic tests will be required for arriving at a definite diagnosis, and subsequent monitoring can be performed using ultrasound, thus obviating the risks associated with radiation generated by CT.
Please cite this article as: García-Alfonso L, Vollmer I, Benegas M, Sánchez M. Ecografía con contraste en el diagnóstico de la atelectasia redonda: a propósito de un caso. Arch Bronconeumol. 2018;54:113–114.