The prevalence of comorbidity in Europe is high with a large proportion of patients aged 60 years and older presenting multiple chronic diseases.1 The management of patients with several comorbidities is challenging due to their frailty and increased risk of mortality. This management is more complex when patients acquire an acute infectious disease. Patients infected with SARS-CoV-2 have different levels of severity of the COVID-19.2 Most of them do not need hospital admission. However, there is a large number of patients that will need advanced care. Just as the necessity of hospitalized care increases with age, so does the prevalence of comorbidities.
The presence of comorbidities in patients hospitalized with COVID-19 is common and may negatively affect their prognosis.3–5 Previous studies have shown that pre-existing diabetes, cardiovascular or chronic kidney diseases can increase the risk of developing severe COVID-196 whereas the increase in mortality was mostly associated with cardiovascular diseases. These studies, however, have not addressed patients older than 59 years, with this group being of special interest due to its high prevalence of comorbidities. Therefore, our main objective is to analyze whether the type of comorbidities increased the risk of hospital mortality in patients with COVID-19 aged 60 years and older treated at the PSMAR (Parc de Salut Mar) university hospital in Barcelona, Spain.
We performed a retrospective evaluation of prospectively collected data from the PSMAR clinical records. This study was approved by the Ethics Committee of PSMAR in 2020. We included patients ≥60 years who had been hospitalized and discharged (alive or dead) from COVID-19 between 23rd February and 12th May of 2020 in the PSMAR. The PSMAR batches four health centres serving a population of approximately 350,000 inhabitants. Included patients had a diagnosis of COVID-19 from the Minimum Basic Data Set that collects the diagnosis leading to admission, and up to 10 comorbidities per patient. Diagnoses are coded according to the International Classification of Diseases 10th edition. We confirmed that patients had a positive result on polymerase chain reaction testing of a nasopharyngeal sample and/or a clinically/radiologically diagnosis of COVID-19. Patients were not followed after discharge but COVID-19 related early readmissions were considered as part of the COVID-19 course. Patients discharged alive directly from the emergency room were excluded.
We evaluated gender, age (60–74, 75–84, or ≥85 years), and the presence of the following comorbidities at the time of hospital admission: hypertension, heart failure, obesity, diabetes, chronic respiratory disease (chronic obstructive pulmonary disease or asthma), malignancy, chronic kidney disease (including kidney transplantation), and chronic liver disease. Mortality was recorded at hospital discharge.
After describing the clinical characteristics, we evaluated differences in the categories stratifying for those patients who died and those who did not using the Mann–Whitney's-U test or Chi-Square test. We used independent logistic regression models to estimate crude and adjusted odds ratios (aOR) of dying and its 95% confidence interval (95%CI) for each comorbidity adjusting by age and gender. All statistical tests were two-sided. P values less than .05 were considered statistically significant.
We included 834 COVID-19 patients aged 60 years and older. 53.5% were women, with an average age of 78.2 (SD=9.8) years, and hospital mortality of 23.5%. The prevalence of patients with at least one comorbidity was 81.9%. Hypertension was the most frequent (64.6%), followed by chronic kidney disease (29.3%), diabetes (28.1%), chronic respiratory disease (17.1%), heart failure (11.9%), obesity (6.6%), malignancy (5.4%), and chronic liver disease (2.3%).
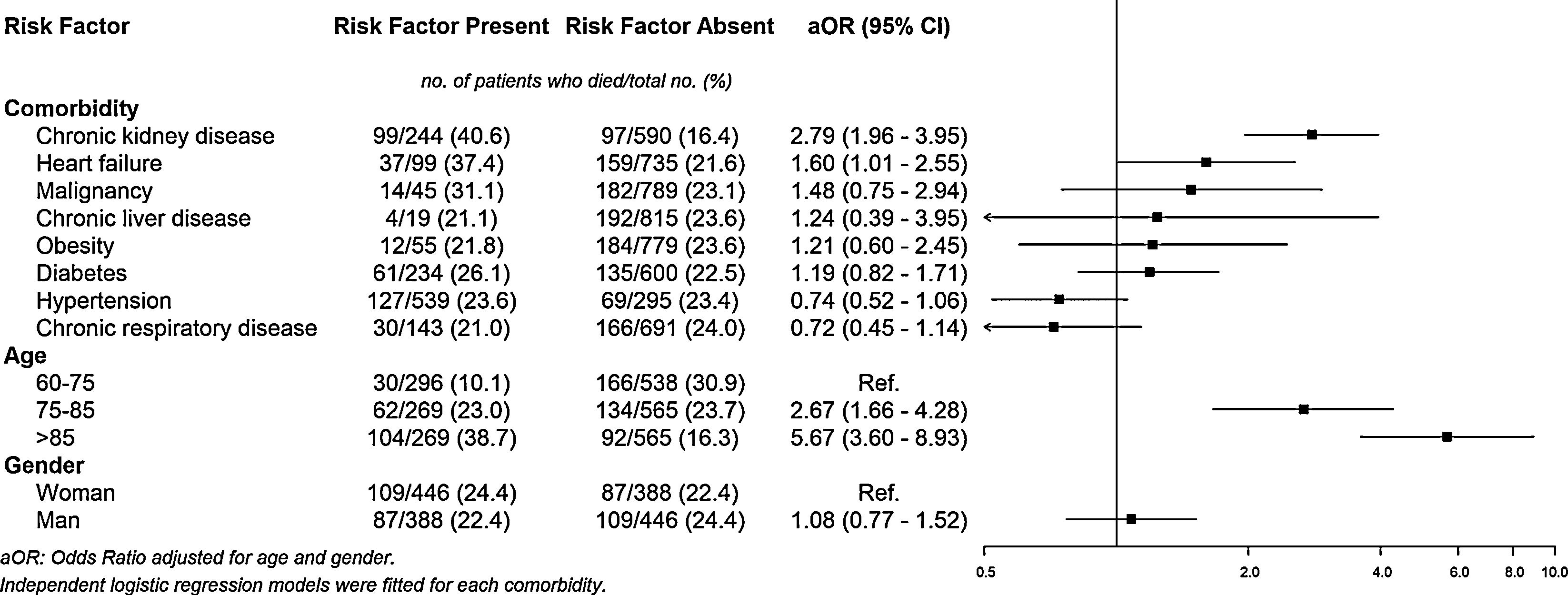
As expected, patients who died were older in average (84 vs. 77 years; P< .001). There was not significant difference in mortality by gender (maleOR=0.89, 95%CI=0.65–1.23). An increase in age increased the risk of dying. Adjusted by gender, the OR (95%CI) were: <75 years=Reference; 75–85 years=2.67 (1.66–4.28); and >85 years=5.67 (3.60–8.93). Adjusted by age and gender, the aOR for hospital mortality was 2.79 (CI95%=1.96–3.95) and 1.60 (CI95%=1.01–2.55) for patients with chronic kidney disease and heart failure, respectively. Patients with malignancy (aOR=1.48, CI95%=0.75–2.94), chronic liver disease (aOR=1.24, CI95%=0.39–3.95), obesity (aOR=1.21, CI95%=0.60–2.45), and diabetes (aOR=1.19, CI95%=0.82–1.71) also presented higher aORs for dying than those without, although these results were not statistically significant. The presence of hypertension and chronic respiratory disease was not associated with hospital mortality (Fig. 1).
In our population of COVID-19 hospitalized patients aged 60 years and older, the presence of pre-existing comorbidities such as heart failure and chronic kidney disease was associated with an increased risk of hospital mortality. We also confirmed that COVID-19-related mortality increased with age. Conversely, we were not able to confirm the association of malignancy, chronic liver disease, obesity, or diabetes with in-hospital mortality but a potential increase in risk was observed. Unexpectedly, the odds ratios for dying of patients with hypertension or chronic respiratory disease were lower than one.
In agreement with previous international studies,6,7 we found that patients with heart failure and chronic kidney disease were more likely to die for COVID-19 than patients without these conditions. It has been suggested that both the direct SARS-CoV-2 infection and the immunologic human response could destabilize pre-existing myocardial and kidney illnesses. Complications, such as acute cardiac8 or kidney9 injuries may, therefore, most frequently occur in patients with these underlying comorbidities leading to an increased risk of death.
The main limitations of this study derive from the modest number of included patients and the information available from the clinical records. Also, we could not address the effect of inpatient treatment or procedures performed during hospitalization. Finally, our analyses were not extended beyond discharge but mortality after this is likely to be small.
In conclusion, in a population of COVID-19 patients aged 60 years and older, the presence of comorbidities such as heart failure and chronic kidney disease is associated with an increased risk of hospital mortality. The mechanisms that underlie the development of severe COVID-19 in patients with pre-existing comorbidities are still poorly understood and warrant further investigation.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.