We report on a 20-year-old woman diagnosed with pulmonary embolism (PE) and right subclavian vein thrombosis attributable to stasis caused by right clavicular prominence. At the 10-months follow-up, the patient had developed chronic thromboembolic pulmonary hypertension (CTEPH), and treatment was begun with a dual endothelin receptor antagonist. Very few cases of deep venous thrombosis of upper limb have been reported in relation to anatomical abnormalities. This case is also exceptional because the patient developed a chronic thromboembolic pulmonary hypertension, whose incidence is estimated at 0.5% of all symptomatic PE.
Se presenta el caso de una mujer de 20 años diagnosticada de tromboembolismo pulmonar (EP) y trombosis de la vena subclavia derecha atribuible a la estasis provocada por la prominencia clavicular derecha. En el seguimiento a los 10 meses la paciente desarrolló una hipertensión pulmonar tromboembólica crónica (HPTEC), instaurándose tratamiento con un antagonista dual del receptor de endotelina. Se han descrito muy pocos casos de trombosis venosa profunda de miembro superior debidos a alteraciones anatómicas. Lo excepcional del caso es que, además, la paciente desarrolló una hipertensión pulmonar postembólica crónica, cuya incidencia se estima del 0,5% del total de los EP sintomáticos.
Upper-extremity deep vein thrombosis (UEDVT), although much less prevalent than lower-extremity deep vein thrombosis, may be accompanied by pulmonary embolism (PE) in up to 15% of cases.1 Since the 1970s, the incidence of UEDVT has increased, fundamentally due to the use of central venous catheters (CVC) and pacemakers.2 The incidence of chronic thromboembolic pulmonary hypertension (CTEPH), defined as pulmonary arterial pressure higher than 25mmHg (measured by right catheterization) that persists 6 months after the diagnosis of PE, occurs in 2%–4%,3,4 although these numbers could be underestimated based on other clinical observations.5
Clinical ObservationWe present the case of a 20-year-old woman, waitress, who came to our consultation due to symptoms of dyspnea, swelling of the upper right extremity and syncope. She is an active smoker of 15 cigarettes/day, and her medical history included rhinoconjunctivitis and bronchial asthma.
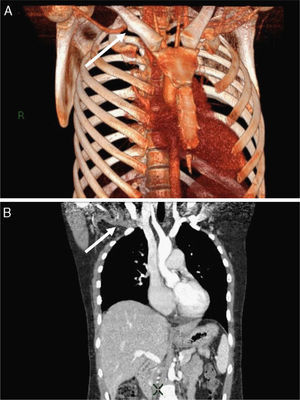
The patient began the previous month with dyspnea upon moderate exertion. When she came to the emergency room, she presented dyspnea at rest, weakness, asthenia and she reported having fainted. Upon examination, she presented: BP: 120/80mmHg; HR: 110bpm and O2: 95%, without supplementary O2. We observed an increased perimeter of the upper right extremity, which was painful to the touch and presented no signs of hardening. The analysis presented biochemical, hepatic, renal, hemogram and coagulation profiles within the normal limits, except for D-dimer: 2500ng/ml. Chest radiography presented no significant findings. Thoracic CT angiogram showed intraluminal filling defects in the segmental arteries of both basal pyramids, upper lobes, middle lobe and lingula. Given the presence of bilateral PE and data showing clinical instability, we decided to admit the patient in the Intensive Care Unit (ICU) and to perform fibrinolysis with rt-PA. Later, CT was done of the neck, chest, abdomen and pelvis (Fig. 1A and B), and a bone spur was observed at the level of the right clavicle that was compressing the right subclavian vein, partially interrupting the venous return. Hypercoagulability studies were negative. The patient underwent resection of the clavicular bone spur, section of the anterior scalene muscle and reconstruction of the clavicular periosteum. Complications during the post-surgical period included post-thrombotic syndrome of the right arm and hematoma in the left iliac muscle with left femoral neuropathy secondary to the introduction of the venous catheter. This latter situation conditioned a period of several months of rehabilitation and the use of a wheelchair.
(A) Tridimensional reconstruction where the bone spur is observed at the right clavicle, which is compressing the subclavian vein and partially interrupting the venous return (arrow). (B) Coronal cut with multiplanar reconstruction where the filling defect of the right subclavian vein is observed.
During follow-up in the outpatient consultation, the patient reported continuing with dyspnea upon moderate exertion, despite her limited mobility due to the post-operative complications. Transthoracic echocardiogram 10 months after the initial diagnosis showed data of possible pulmonary hypertension with an estimated systolic pulmonary arterial pressure of 67mmHg, which was confirmed by means of right cardiac catheterization revealing a mean pulmonary arterial pressure of 48mmHg and systolic pressure of 78mmHg. In a control CT angiogram 3 months later, we identified no intravascular filling defects that suggested pulmonary embolism, therefore performing a thromboendarterectomy was dismissed.
Treatment was begun with bosentan (dual endothelin-receptor antagonist). In the last follow-up in the pulmonary outpatient consultation 18 months after the initial episode, the patient continued to have NYHA (New York Heart Association) functional class grade I dyspnea, echocardiographic data showing the persistence of light-moderate hypertension with a systolic arterial pressure of 50mmHg, with good tolerance to bosentan and with mild post-thrombotic syndrome.
DiscussionUEDVT represents 1%–4% of all deep vein thromboses, and it is more frequent in young men between the ages of 27 and 52.6 UEDVT can be classified into 2 etiologies: primary (including the idiopathic cases, those related with exertion or the Paget-Schroetter syndrome and thoracic outlet syndrome); and secondary, caused by the use of central venous catheter (75% of all cases), pacemakers or cancer.
In our patient, we found evidence of a clavicular anatomic malformation as the cause of venous thoracic outlet syndrome (TOS).7 This syndrome is defined as the occlusion or compression of the subclavian vein in the area of the superior thoracic outlet between the clavicle, the first rib, the tendon of the subclavian muscle and the costoclavicular ligament.
In the cases of TOS caused by clavicular malformations (either congenital or due to fracture callus), the bone protrudes and directly compresses the neurovascular structures of the costoclavicular space. A variety of surgical treatments have been described, including callus resection, resection of all or part of the clavicle, resection of the lower surface of the clavicle, corrective osteotomy and scalenectomy. If the clavicular spur or callus does not directly compress the neurovascular structures and the costoclavicular space is wide enough to for the brachial plexus to move freely, then simply a scalene muscle section may be performed.8 In the case of our patient, however, it was necessary to resect the clavicular bone spur and to perform scalenectomy.
The data published over the past 20 years suggest that UEDVT is associated with a significant prevalence of PE, which varies widely in the literature from 2% to 35%.9
The incidence of CTEPH is estimated to be between 0.1% and 0.5% in patients who survive symptomatic PE.10 Nevertheless, more recent studies suggest that this entity is underdiagnosed and therefore the previous numbers were far from the actual incidence.5 It is also possible that the quantity of embolic material that persists in the pulmonary arteries may be related with the increased risk for developing CTEPH. The physiopathology of CTEPH is still not clarified. The most commonly accepted explanation (the embolic hypothesis) is that CTEPH is the result of pulmonary embolism, either single or recurring, that arises from the areas with venous thrombosis.6 However, it has been suggested that CTEPH can be the result of a primary arteriopathy and endothelial dysfunction, similar to that seen in primary pulmonary arterial hypertension (PAH), which causes lung thrombosis in situ. This would explain why more than 60% of patients with CTEPH do not have a history of DVT.11 The progressive remodeling of the small pulmonary arteries in occluded and non-occluded territories favors the possible implication of pulmonary arteriopathy in CTEPH.12
What is exceptional about the case presented are the few documented cases of upper-extremity deep vein thrombosis due to anatomical alterations, which in our patient was also accompanied by PE that evolved into pulmonary hypertension, whose prevalence is also low.
Please cite this article as: Ferrer Galván M, et al. Hipertensión pulmonar tromboembólica crónica debida a trombosis venosa profunda de miembro superior por síndrome del desfiladero torácico. Arch Bronconeumol. 2011:48:61–3.