Aspergilloma is the most frequent cause of lung involvement by Aspergillus (50%). Its incidence is unknown, and the most common predisposing factor is the presence of a cavity previously caused by tuberculosis, observed in up to 70%–80% of cases. The aspergilloma is formed when these cavities are colonized by certain species of Aspergillus, the most common in humans being Aspergillus fumigatus. Systemic or intracavitary antifungal drugs, which have poor penetration into cavitary lesions, only play an adjunct role in treatment and are ineffective in eradicating the microorganism.1 Surgery, therefore, can completely eliminate the cavity and reduce associated complications, although this approach is controversial due to the high incidence of postoperative morbidity and mortality described in the literature.2–4
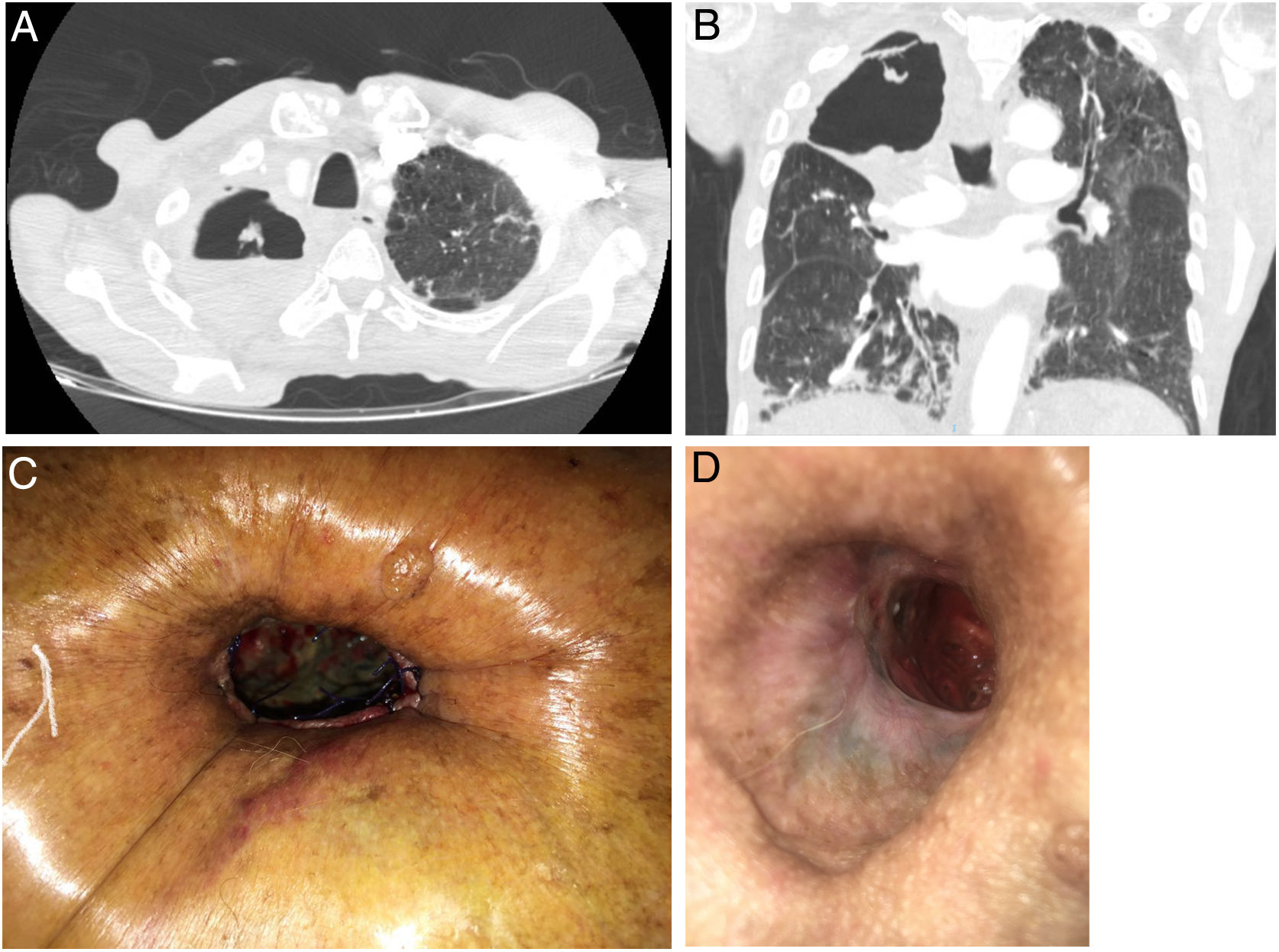
We present the case of a 79-year-old man, recipient of a liver transplant 30 years previously due to chronic HCV-induced liver disease in a situation of chronic rejection. The patient underwent atypical lung resection for tuberculosis in 1970, and presented residual fibrotic lesions in the right lung. He was admitted in 2016 due to hemoptoic expectoration. After sputum smear and culture were found to be positive for mycobacteria, he was diagnosed with infection by Mycobacterium szulgai and treated with rifampicin, clarithromycin and ethambutol for 12 months, with good response and negative sputum. One year later, he was admitted for massive hemoptysis associated with a cavitated lesion in the right upper lobe (Fig. 1A, B) that persisted despite bronchial artery embolization and morphine hydrochloride perfusion. He also presented severe malnourishment that required nutritional support through a nasogastric tube prior to surgery and for several weeks thereafter.
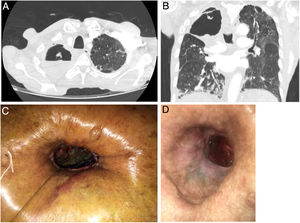
Due to the risk associated with lung resection, the peripheral location of the lesion, and the likelihood of pleural adhesions and mediastinal fibrosis (Fig. 1A, B), we decided to perform cavernostomy in the right upper lobe - a far less aggressive procedure that has been proven effective for the control of infection and hemoptysis in the literature. An incision was made at the level of the second rib and a fragment of bone was resected from the anterolateral portion of that rib. The walls of the cavity were debrided to remove all the necrotic tissue, the interior was cleaned thoroughly and the edges of the incision were invaginated into the cavity. The cavity wound was treated with occlusive dressings of gauze impregnated with amphotericin B applied via the cavernostomy, intravenous amphotericin B was administered for 14 days, and nebulized amphotericin B was maintained after discharge. Aspergillus niger was isolated from the culture of the surgical sample, but postoperative cultures were negative. The patient was discharged after 3 weeks in good clinical condition, and currently continues with daily local treatment of the cavernostomy in the health center and periodic follow-up by the Thoracic Surgery and Pulmonology service.
The main problem encountered during follow-up has been the persistence of air leaks from the cavernostomy (Fig. 1D) that has prevented us from using negative pressure therapies, since they would only worsen the leakage. We also ruled out performing myoplasty to close the cavernostomy, as this procedure would have been impractical due to the patient’s loss of muscle mass. One option we considered was the use of endobronchial valves to obliterate the bronchus or segmental bronchi affected by the persistent air leak; however, the patient refused to undergo additional procedures.
The literature on the surgical treatment of aspergilloma is essentially based on case series. The most frequent indications for surgery are hemoptysis refractory to conservative treatment and diagnosis in asymptomatic patients. The most widely performed procedure in all published series is lobectomy, followed by sublobular resection and bilobectomy or pneumonectomy. Cavernoplasty or cavernostomy is the last option in all reports, and has received little attention in the literature. The postoperative complication rate is 20%–30%, and immediate postoperative mortality is 5%–10%.5–9
Cases series describing intracavitary administration of antifungals and even removal of the aspergilloma using flexible bronchoscopy have been published.10,11
Lung resection, either in the form of pneumonectomy, lobectomy, or wedge resection, is the technique of choice in patients with good baseline status and acceptable surgical risk. Cavernostomy can give adequate control of infection and hemoptysis, and is an option in patients with high surgical risk, such as the case we describe. However, it is not without complications, particularly bleeding, and requires close, long-term monitoring with topical treatment.12
FundingNo funding was received.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Tabales JG, Sardiña DA, Matás CS, Blanco SM, Gómez FG, Villalobos JLL, et al. Tratamiento del aspergiloma pulmonar en paciente de alto riesgo quirúrgico: cavernostomía. Arch Bronconeumol. 2020;56:596–597.