The abnormal calcification of normal lung tissue, known as metastatic pulmonary calcification, is a frequent complication in patients with chronic kidney failure and secondary hyperparathyroidism, especially those in hemodialysis programs.1 It is usually characterized by the presence of numerous calcified nodules from 3 to 10mm in diameter, which are observed on high-resolution computed tomography (HRCT)2,3 as ground-glass opacities that are usually centrilobular, without septal thickening. There is no correlation between the extension of the macroscopic calcifications and clinical symptomatology.4,5 The anatomopathologic samples show intense hematoxylin staining of the alveolar walls and the walls of the small lung vessels and bronchi, with mild-to-moderate fibrosis of the alveolar walls, with no affectation of the adjacent air spaces.
Pleural calcification is often the result of a hemothorax, pyothorax, or an old tuberculous effusion, and it is commonly associated with extensive pleural thickening, either as a continuous wide sheet or multiple small plaques. Another diagnostic possibility is the exposure to asbestos and talc, which show an approximate latency period of 15 years, correlating with the intensity of the initial exposure and the time exposed.
We present the case of a 64-year-old patient who was admitted to our unit for emergency care due to the presentation of persistent right pleural effusion evolving over the period of several months, with neither intercurrent infectious processes nor thoracic pain, nor any symptoms suggesting congestive heart failure.
The patient's personal history included chronic renal insufficiency (without dialysis) with an estimated creatinine clearance of 20% and hypertensive heart disease. Complementary tests done upon admittance showed normocytic normochromic anemia and renal failure with creatinine 3.9mg/dl. The patient presented reduced calcium and increased phosphorus levels, which, together with high levels of parathyroid hormone (177pg/ml; normal levels: 15–88pg/ml), was consistent with secondary hyperparathyroidism. Chest radiography revealed cardiomegaly with growth of the left cavities and moderate right pleural effusion. Diagnostic thoracocentesis showed biochemical characteristics of exudate with limited lymphocytes. Thoracic CT revealed mild cardiomegaly with right pleural effusion, no pleural thickening, and calcium deposits on the visceral pleura.
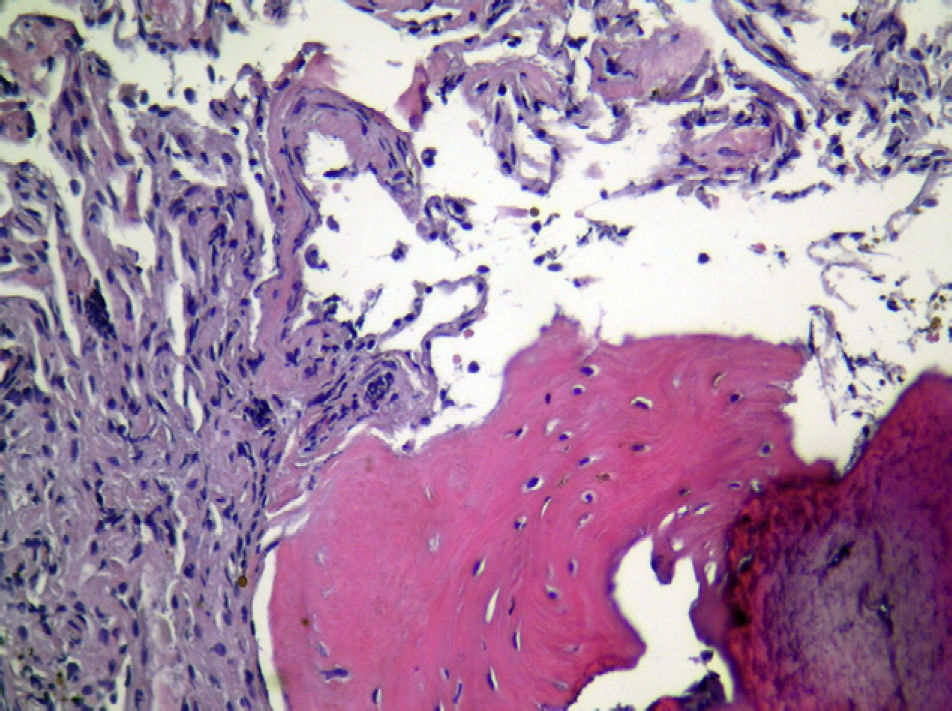
Given these findings, video-assisted thoracoscopy was performed, where diffuse inflammatory signs were observed in the two pleural cavities, as well as plaques reminiscent of mother-of-pearl that were hard to the touch, both in the parietal pleura as well as the visceral pleura. The samples remitted made evident the existence of areas of pleural thickening with the formation of bone tissue (Fig. 1) and no evidence of infiltration by tumor cells or of calcium deposits on the walls of the adjacent alveoli, which were free.
Metastatic pulmonary calcification is a rare clinical entity that has been reported on a limited number of occasions in the medical literature.6 It usually appears in a context similar to that of this case, requiring a differential diagnosis with other clinical entities that run their course with pleural thickening and calcification.
Please cite this article as: Alcázar Navarrete B, et al. Calcificación metastásica pleural secundaria a hiperparatiroidismo secundario. Arch Bronconeumol. 2011;47:576.